FInal 2024 ACA Open Enrollment Deadline is MIDNIGHT TONIGHT in most states. Here's 12 important things to remember:

The 2024 ACA Open Enrollment Period (OEP) is STILL ongoing in 49 states +DC.
This is the best OEP ever for the ACA for several reasons:
- The expanded/enhanced premium subsidies first introduced in 2021 via the American Rescue Plan, which make premiums more affordable for those who already qualified while expanding eligibility to millions who weren't previously eligible, are continuing through 2025 via the Inflation Reduction Act;
- A dozen states are either launching or expanding their own state-based subsidy programs to make ACA plans even more affordable for their enrollees;
- Millions more Americans who weren't previously eligible for ACA subsidies (even with the expanded ARP/IRA enhancements) are now eligible via the Biden Administration's closure of the so-called "Family Glitch."
And remember, millions of people will be eligible for zero premium comprehensive major medical policies.
If you've never enrolled in an ACA healthcare policy before, or if you looked into it a few years back but weren't impressed, please give it another shot now. Thanks to these major improvements it's a whole different ballgame.
Here's some important things to know when you #GetCovered for 2024:
1. DON'T DELAY; GET COVERED SOONER RATHER THAN LATER!
The official 2024 Open Enrollment Period runs from November 1st through January 16th in most states, but there are some exceptions at both ends.
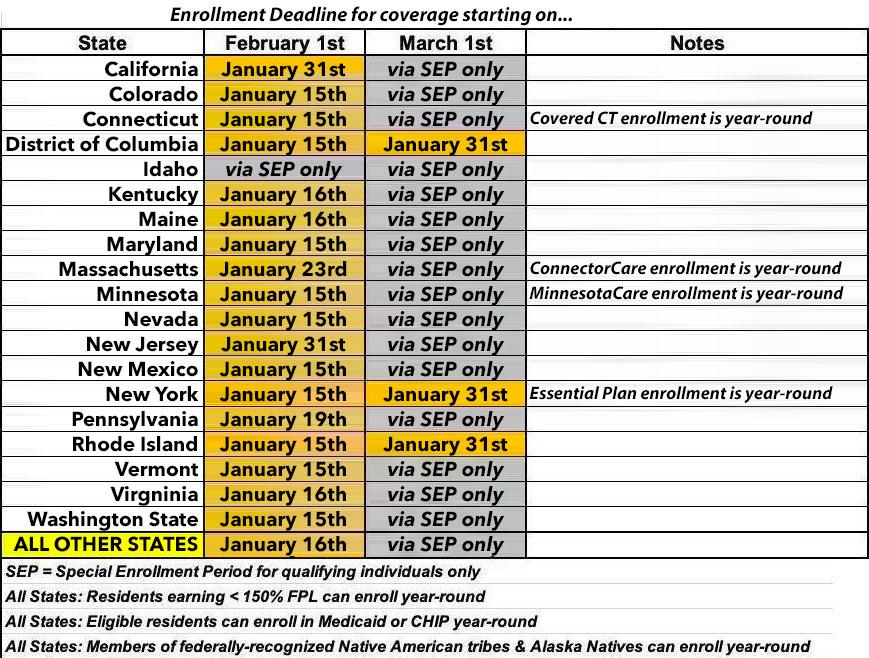
At the opposite end, most states have their final deadline on January 15th or 16th, but several states have later final deadlines. Here's a summary of the deadlines to sign up for 2024 ACA healthcare coverage, and when that coverage will start. These are subject to last-minute extensions:
UPDATE 01/10/24: Pennsylvania has extended the final deadline to enroll to January 19th.
UPDATE 01/16/24: Connect for Health Colorado has posted the following notice:
If you were unable to complete your enrollment by January 15, you may still be able to get covered for February 1st. Call us at 855-752-6749 no later than 6pm on January 17th, or contact your Broker/Assister.
UPDATE 01/16/24: Vermont Health Connect has posted the following notice:
Did you miss the 1/15 deadline to enroll in a 2024 health plan? You might still be eligible for a plan starting 2/1/24 if you try TODAY ONLY! Our Customer Support Center is open from 8am-6pm at 855-899-9600. OR Complete your online application today at www.VermontHealthConnect.gov. Click on the orange LOG IN button. Choose a 2024 health plan and confirm enrollment through the day, up to midnight.
Note that residents of any state earning less than 1.5x the Federal Poverty Level are eligible to enroll year-round, as are members of federally-recognized Native American tribes or Alaska Natives. In addition, people who are eligible for Medicaid or the Children's Health Insurance Program (CHIP) are eligible to enroll in those programs year-round.
There are also several state-specific programs which allow eligible enrollees to do so year round. These include "Covered Connecticut" in Connecticut; "ConnectorCare" in Massachusetts; MinnesotaCare in Minnesota and the Essential Plan in New York. I'll discuss each of these in more detail below.
If you want to enroll outside of the dates above, you may have to qualify for a Special Enrollment Period (SEP). Qualifying Life Experiences (QLEs) which make you eligible for a SEP include things like:
- Losing employer-sponsored healthcare coverage
- Getting married or divorced
- Giving birth/adopting a child
- Turning 26 and having to move to your own policy
- Losing eligibility for Medicaid or CHIP
- Moving out of your current rating area
However, if your income is less than 150% FPL, or if you're a member of a federally-recognized Native American tribe or are an Alaskan Native, you can enroll in an ACA exchange plan year-round regardless of what state you live in.
In addition, if you're eligible for Medicaid; the Children's Health Insurance Program (CHIP); Massachusetts' "ConnectorCare" program; Minnesota's "MinnesotaCare" program; or New York's "Essential Plan" program, you can enroll year-round.
2. ONLY ENROLL VIA AN OFFICIAL ACA HEALTH EXCHANGE OR AN AUTHORIZED ENROLLMENT PARTNER.
ACA financial subsidies are available to millions more Americans than they used to be...but they're only availalble to eligible enrollees who sign up through an official ACA exchange or an authorized 3rd-party exchange entity, known as an Enhanced Direct Enrollment (EDE) entity.
There's a ton of junk plans and scam artists out there, especially these days. Fraudulent plans are being hawked endlessly via both robocalls, spam emails and fly-by-night websites. If you're enrolling online, make sure to use one of the official ACA exchange websites:
- CALIFORNIA: Covered California
- COLORADO: Connect for Health Colorado
- CONNECTICUT: Access Health CT
- DISTRICT OF COLUMBIA: DC Health Link
- IDAHO: Your Health Idaho
- KENTUCKY: kynect
- MAINE: CoverME.gov
- MARYLAND: Maryland Health Connection
- MASSACHUSETTS: MA Health Connector
- MINNESOTA: MNsure
- NEVADA: Nevada Health Link
- NEW JERSEY: Get Covered NJ
- NEW MEXICO: beWellnm
- NEW YORK: NY State of Health
- PENNSYLVANIA: Pennie
- RHODE ISLAND: HealthSource RI
- VERMONT: VT Health Connect
- VIRGINIA: VA's Insurance Marketplace (new!)
- WASHINGTON STATE: WA Healthplan Finder
- As for EDEs, it's important to note that some of these may also sell non-ACA compliant plans. The largest EDE, HealthSherpa, only sells on-exchange ACA-compliant policies. Full disclosure: They advertise on this website.
As noted above, VIRGINIA just launched their brand-new state-based ACA exchange a few weeks ago.
Note: While some insurance carrier websites are also hooked into the federal exchange via an EDE, they (understandably) only list their own plans. I still recommend only using one of the websites listed above. Remember, whether via an official exchange site or an EDE, you have to enroll on-exchange to be eligible for financial help!
On a related note...
3. IF YOU'RE ENROLLED OFF-EXCHANGE, SEE IF YOU CAN ENROLL ON-EXCHANGE INSTEAD.
As far as I can figure, somewhere around 2 million Americans are still enrolled in OFF-exchange, ACA-compliant individual market policies. Historically, the main reason for this has been that they didn't qualify for financial help, so didn't see the point of filling out any additional forms by enrolling on-exchange.
The reality, however, is that many of these off-exchange enrollees may have been eligible for ACA subsidies after all if they had enrolled in the exact same plan but had done so via their ACA exchange instead of directly through the carrier...and thanks to the dramatically improved subsidies of the American Rescue Plan/Inflation Reduction Act (plus supplemental subsidies in some states), many of these people are leaving thousands of dollars in savings on the table if they don't make the switch!
Again: If you weren't eligible a few years ago or even last year, check again this year; you may be in for a very pleasant surprise!
On average, full-price/unsubsidized ACA premiums went up around 3.5% overall in 2022 and around 7% in 2023. For 2024 they're going up another 6.6% or so, with wide ranges from state to state, carrier to carrier and plan to plan.
I can't repeat this enough times: If you enroll off-exchange, there's a good chance you'll be leaving potentially thousands of dollars in savings on the table.
4. MILLIONS OF AMERICANS CAUGHT IN THE "FAMILY GLITCH" MAY NOW BE ELIGIBLE FOR UP TO THOUSANDS OF DOLLARS IN SAVINGS!
As I explained here, due to how the U.S. Treasury Dept. and the Obama Administration interpreted an obscure provision of the Patient Protection & Affordable Care Act regarding employer coverage affordability thresholds, there are several million people who really should have been eligible for ACA subsidies for years now but who haven't been.
The very short version of the problem is this:
- Let's say you have healthcare coverage for yourself only through your employer, and you only have to pay, say, 5% of your annual household income for your premiums
- However, you're married with two kids, and adding each of them would tack on another 5% in premiums apiece. Covering all four of you would cost 20% of your annual household income, ouch.
- Because your individual premiums come in at less than ~9.12% of your income, the rest of your family doesn't qualify for ACA subsidies even though the premiums for the family as a whole costs far more than the maximum amount you'd otherwise have to pay for an ACA exchange plan.
Thankfully, since 2022, this is no longer an issue for most of these folks.
5. OTHERS WHO DIDN'T USED TO QUALIFY FOR FINANCIAL HELP NOW QUALIFY AS WELL!
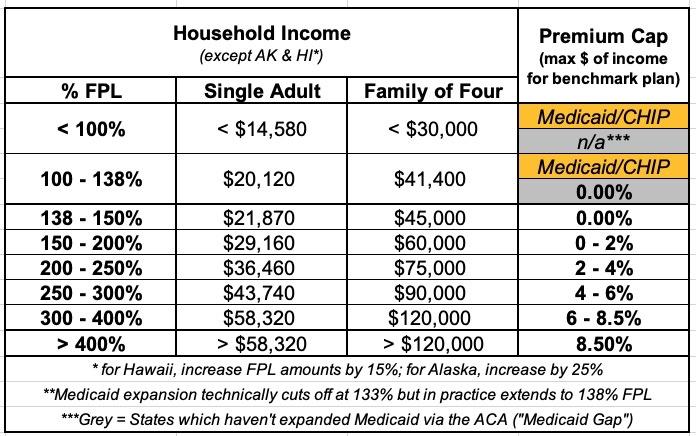
Before I get into this, it's important to understand what the Federal Poverty Line (or FPL) is. 100% FPL depends on how many people live in your household. For a single adult with no dependents, it's $14,580/year; for a family of four, it's $30,000/year. These amounts increase a bit each year to account for inflation.
Prior to the American Rescue Plan/Inflation Reduction Act, ACA subsidies were limited (on a sliding income scale) to enrollees earning between 100 - 400% FPL (roughly $58,000/year for one person or $120,000/year for a family of four this year). If you earned more than 400% FPL, however, you had to pay full price no matter how expensive the premiums were.
Thanks to the ARP/IRA, however, the ACA's infamous "Subsidy Cliff" has been killed at last through at least the end of 2025.
This means two extremely important things:
- First: Households earning less than 400% of the Federal Poverty Line (FPL) are now eligible for more generous financial assistance than they were pre-ARP/IRA.
- Second: Millions of people who earn more than 400% FPL, who weren't eligible for any financial help pre-ARP/IRA, are now eligible for financial help after all, which can mean thousands of dollars in savings for many of them.
Here's a table laying out the percent of your household income which you're restricted to paying for the benchmark Silver plan in your area for 2024:
6. ELEVEN STATES ARE OFFERING *ADDITIONAL* SAVINGS *ON TOP OF* THE EXPANDED ARP SUBSIDIES!
In addition, several states have special programs and/or additional savings on top of the enhanced federal subsidies which can save many lower-income enrollees even more!
- CALIFORNIA: STATE-ENHANCED COST SHARING REDUCTION PROGRAM
Over 600,000 CA residents are expected to benefit from the new program which eliminates deductibles for all CoveredCA enrollees earning up to 250% FPL while also dramatically reducing co-pays & other cost sharing for those earning 150 - 250% FPL. This effectively turns all CSR Silver plans into Secret Ultra Platinum plans.
CoveredCA also plans on automatically upgrading ~35,000 enrollees into High CSR plans to save them money, while also covering the $1/month abortion rider fee for every enrollee.
- COLORADO: HEALTH INSURANCE AFFORDABILITY FUND
Over 50,000 CO residents are already benefitting from this program, which again upgrades enrollees earning up to 250% FPL to the same Platinum plan status as those earning less than 150% FPL by reducing out-of-pocket expenses (deductibles, co-pays, etc.) even further. An additional 22,000 residents are expected to become eligible for the program this year.
In addition, up to 11,000 undocumented immigrants earning up to 300% FPL who aren't eligible for federal subsidies are eligible for state-based premium subsidies as well via Colorado's unique OmniSalud program.
- CONNECTICUT: COVERED CONNECTICUT PROGRAM
This program, which has around 17,000 Ct residents enrolled, raises the actuarial value of ACA plans to a stunning 100% (ie, no cost sharing at all) for all Silver CSR enrollees earning up to 175% FPL. This even includes no-cost dental insurance and non-emergency medical transportation.
- MINNESOTA: MINNESOTACARE
Over 110,000 Minnesota resents with household income is up to 200% FPL are enrolled in the states expanded MinnesotaCare Basic Health Plan program.
Minnesotacare features $0 premiums for households earning up to 160% FPL and $4 - $28 premiums on a sliding scale for households earning 160 – 200% FPL. Children up to 20 years old have no cost sharing, and adults 21+ only pay $100 for ER visits and have very low co-pays for other typical services.
- MARYLAND: YOUNG ADULT SUBSIDY PROGRAM
Around 43,000 Maryland residents are enrolled in this program. If at least one of the enrollees in your household is between the ages of 18 - 37 and your household income is up to 400% FPL, they may qualify for additional premium savings. It reduces net premiums after federal subsidies are applied by an additional 2.5 percentage points for enrollees from 18-33 and by smaller amounts over that on a sliding scale.
- MASSACHUSETTS: CONNECTORCARE
Around 128,000 MA residents are enrolled in ConnectorCare plans, which are special Qualified Health Plans (QHPs) only available to MA Health Connector enrollees who earn up to 500% FPL (previously 300% FPL). They feature $0 deductibles, low out-of-pocket caps, low co-pays and nominal (or even $0) premiums. An additional 50,000 Bay Staters are expected to be eligible this year!
- NEW JERSEY: NJ HEALTH PLAN SAVINGS PROGRAM
This program, which nearly every enrollee at Get Covered NJ benefits from to some degree, automatically further reduces premiums for eligible enrollees who earn up to 600% FPL. These are flat “wraparound” subsidies provided on a monthly basis as a supplement to the federal APTC subsidies.
- NEW MEXICO: HEALTH CARE AFFORDABILITY FUND
This program was introduced last year; it benchmark Silver premiums for enrollees earning up to 200% FPL down to $0, while also reducing them by lesser amounts for enrollees earning between 200 - 400% FPL. It also dramatically upgrades the cost sharing reduction subsidiesm while rebranding Silver CSR plans as “Turquoise Plans” for easier consumer marketing.
- NEW YORK: THE ESSENTIAL PLAN
A stunning 1.3 MILLION New Yorkers are now enrolled in this Basic Health Plan program; similar to MinnesotaCare, residents earning up to 200% FPL are eligible for the Essential Plan, which has been expanded to the point that enrollees pay NO premiums and have NO deductibles! In addition, enrollees earning up to 150% FPL pay almost nothing in cost sharing, which is pretty nominal for those earning 150 - 200% FPL.
- VERMONT: VERMONT PREMIUM ASSISTANCE
Available to Vermont residents (around 15,000 are enrolled at the moment) earning up to 300% FPL, VPA subsidies are unusual in that they reduce net premiums by 1.5 percentage points...which means that some low-income enrollees are technically paying negative premiums. In reality, the "excess" subsidies just go to cover any premiums for services not covered by federal subsidies (no, you don't actually get paid for enrolling).
- WASHINGTON STATE: CASCADE CARE SAVINGS
Available for enrollees earning less than 250% FPL who enroll in Silver or Gold “Cascade Care” plans (Cascade Care plans are Washington’s quasi-”public option” ACA policies). Further reduces net premiums down to as low as $0/month; most pay $10/month or less. Cascade Care plans have deductibles/co-pays around $1,000 lower than non-Cascade Care Silver plans.
7. MILLIONS OF PEOPLE ARE ELIGIBLE FOR FREE "SECRET PLATINUM" PLANS (LABELED AS SILVER)!
As I explain in detail here, if your household earns less than 200% FPL in any state (around $29,000/yr if you're single; around $60,000/yr for a family of four), make sure to choose a SILVER plan! Thanks to the ACA's Cost Sharing Reductions (CSR) system, you'll receive additional financial help which will lower your deductible, co-pays and coinsurance so much it effectively transforms Silver plans into Platinum plans!
Furthermore, thanks to the expanded ARP/IRA subsidies, the premiums for these "Secret Platinum" plans are literally nothing for anyone earning under 150% FPL and max out at just 2% of your annual income from 150 - 200% FPL! (As noted above, in some states you may not have to pay a dime in premiums for a Silver plan even if your income is as high as 200% FPL).
8. VIA PREMIUM ALIGNMENT & SILVER LOADING, SOME SUBSIDIZED ENROLLEES MAY BE ABLE TO GET FREE GOLD PLANS!
As I explained here, due to a long, strange series of events, subsidized enrollees earning 200% FPL or more may end up getting a Gold plan for less than Silver, or a Bronze plan for free!).
In 2021, David Anderson ran an analysis and finds that there were 820 counties where at least one Gold plan was priced lower than the benchmark Silver plan even at full price! Once you add Silver Loading into the mix, this means many people will qualify for a ZERO-PREMIUM GOLD plan even if they earn over 200% FPL!
This is especially true in states which have fully embraced both Silver Loading and Premium Alignment, including Colorado, Maryland, New Mexico, Pennsylvania and Texas (both Illinois and New Jersey have bills in committee to do this as well; I hope Michigan will do so soon!)
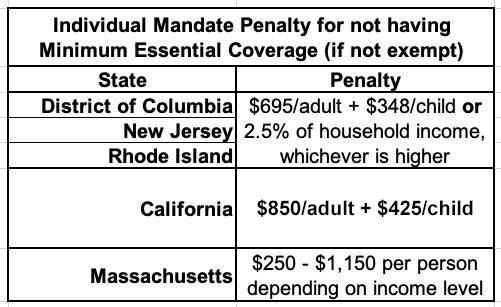
9. THE INDIVIDUAL MANDATE IS STILL AROUND IN FIVE STATES!
The single most controversial part of the Patient Protection & Affordable Care Act was the Shared Responsibility Provision, commonly known as the "Individual Mandate Penalty." In essence, all American citizens who didn't qualify for an exemption were required to either have ACA-compliant healthcare coverage (this could include Medicare, Medicaid, CHIP, qualifying Employer-Sponsored healthcare policies, or ACA exchange plans) or they would be charged a financial penalty for not having qualifying coverage.
The federal ACA individual mandate was reduced to nothing in 2019, so it isn't an issue any longer...but there are actually five states which have since reinstituted their own healthcare coverage requirement:
- CALIFORNIA
- DISTRICT OF COLUMBIA (I know, it's not actually a state...yet)
- MASSACHUSETTS
- NEW JERSEY
- RHODE ISLAND
In CA, DC, NJ & RI, the penalty either identical or very close to the old federal penalty. Massachusetts uses their own formula. The financial penalty for not having coverage (assuming you don't qualify for an exemption) will be charged when residents file their 2022 state taxes in spring 2023.
10. SOME CARRIERS HAVE EITHER NEWLY ENTERED OR EXITED DIFFERENT STATES
Every year sees churn on the ACA markets as new carriers enter or expand their coverage areas to more counties/states...or as currently-participating carriers pull out of them. In addition, existing carriers often add new plans or phase out current ones. Here's just some of the changes for 2024:
New carriers are joining the market in these states:
- California: Inland Empire
- Colorado: SelectHealth
- Delaware: Celtic
- Indiana: Aetna Health
- Maryland: Aetna Health
- Nevada: Imperial Insurance Co; Molina Healthcare of NV
- New Jersey: UnitedHealthcare
- New Mexico: UnitedHealthcare of NM
- Oklahoma: Taro Health
- Pennsylvania: Jefferson Health Plans
- South Carolina: UnitedHealthcare
- Utah: Aetna Health; Imperial Health Plan of the SW
- Wisconsin: UnitedHealthcare
- Other carriers are leaving states, such as Bright and Friday Health Plans (both of which went belly-up last/this year), or Oscar Health leaving California.
Any time a carrier reduces their participation in a given county or state it means that anyone currently enrolled in their policies will either be automatically "mapped" to a similar plan with a different carrier or they have to actively seek out a new policy to enroll in.
11. STANDARDIZED PLANS ARE BACK!
I debated a long time on whether to make this its own separate category or not.
Several states such as California and Massachusetts already mandate "Standardized" ACA policies. This means that every plan offered within a given metal level category (Bronze, Silver, Gold, Platinum) has to have the same cost sharing across the board. That is, co-pays, deductibles, etc. have to be the same. This simplifies the decision process for enrollees by allowing them to focus on premiums and networks instead of having to sweat the co-pays for 80 different services.
Standardized plans were offered by some carriers on the federal ACA exchange a few years back, but it was pretty scattershot since they didn't have to. All carriers offering plans on HealthCare.Gov now have to include standardized plans at every metal level.
Related to this, new for 2024: HC.gov is limiting the total number of plans offered by each carrier to no more than 4 non-standardized plans per network type, metal level, service area & dental/vision benefit. This is being done in an attempt to reduce the mountain of confusing, virtually-identical plans offered on the exchange, although honestly that still allows for something like 24 plans per metal level per carrier. Still, it's a start; next year it will be reduced to 2 plans per option, which should help reduce the clutter.
So why was I hesitant to give standardized plans (aka "Easy Pricing") their own bullet point on this list? Because unlike CA & MA, the "Easy Pricing" plans which have to be included on HealthCare.Gov's offerings are in addition to the dozens (or even hundreds) of existing "non-standardized" plans already offered. This means that instead of simplifying the shopping experience, it could actually make it more confusing for some people.
All of this can get understandably confusing to the point that it becomes overwhelming. Fortunately...
12. THE NAVIGATOR PROGRAM IS BACK AT FULL STRENGTH, BABY!
Years ago, the Trump Administration effectively gutted both the ACA's marketing/outreach budget (slashing it down by 90%) as well as its "Navigator" program, causing dozens of organizations around the country devoted to helping ACA enrollees find their way through the confusing world of health insurance enrollment (as well as those needing guidance to get into Medicaid, CHIP and other healthcare programs).
Thankfully, those days are no more: The Biden Administration reversed this damage, quadrupling the number of ACA Navigators to over 1,500 and increasing the grant program to nearly $100 million this year.
The news is even better for underserved communities...those who need help the most:
Navigators serve an important role in connecting communities to health coverage, including communities that historically have experienced lower access to health coverage and greater disparities in health outcomes. Entities and individuals cannot serve as Navigators without receiving federal cooperative agreement funding, authorized in the Affordable Care Act, to perform Navigator duties.
To find authorized local help, search here. If you live in a state with its own ACA exchange you'll be redirected there.
UPDATE 1/01/24: Now that we're into January, the last item on the list is mostly moot, but I'm keeping it listed for future reference.
13. *DON'T* LET YOURSELF BE PASSIVELY AUTO-RENEWED!
It's always been a good idea to actively shop around the ACA marketplace each Open Enrollment Period to see whether there's a better value for the upcoming year, but it's even more important now.
Between the massively expanded & enhanced subsidies thanks to the ARP/IRA, the dramatic increase in carrier participation in many states, the supplemental financial assistance being provided to many enrollees in nearly a dozen states, the seemingly counterintuitive pricing structure caused by "Silver Loading" and a host of other factors, you should absolutely NOT let yourself be "auto-renewed" this year!
My friend & colleague Louise Norris lists some important reasons for this:
In most states, you’ll have limited opportunities to pick a new plan after your coverage is auto-renewed. The auto-renewal process happens right after December 15, for people who haven’t manually renewed or selected a new plan. Since open enrollment now extends into January in nearly every state, enrollees in most states have until at least January 15 to pick a new plan if they ended up deciding that the auto-renewed option wasn’t the best choice after all.
Your subsidy amount will generally change from one year to the next. If your subsidy gets smaller, auto-renewal could result in higher premiums next year. If the cost of the benchmark plan changes, premium subsidy amounts in that area will also change. The benchmark plan for 2023 may or may not be the same plan that held the benchmark spot in 2022.
If you receive a subsidy, auto-renewal could be dicey even if the subsidy amount isn’t declining. If you rely on auto-renewal (as opposed to manually renewing and completing the financial eligibility determination process for the coming year), the exchange can renew your plan without a premium subsidy in certain circumstances. This includes situations in which you didn’t give the exchange permission to access your financial information in subsequent years, or if you failed to reconcile your premium subsidy on the prior year’s tax return.
If your plan is being discontinued at the end of 2022, auto-renewal will result in the exchange or your insurer picking a new plan for you. They will try to assign you to the plan that most closely matches the coverage you had in 2022, but selecting your own new plan is a better option.
Auto-renewal might result in a missed opportunity for a better value. Even if the plan you have in 2022 represented the best value when you selected it, there may be different plans available for 2023. Provider networks and benefit structures can change from one year to the next, as can premiums. You might still decide that renewing your 2022 plan is the best option for 2023. But it’s definitely better to actively make that decision rather than letting your plan auto-renew without considering the other available options.
Note that this doesn't necessarily mean that you shouldn't actively renew your existing plan--it may turn out that sticking with the same healthcare policy really is your best bet after all. Just don't assume that's the case, because even if nothing changes at your end (same income, same household size, etc.), the plans, premiums, networks and especially the subsidies you're eligible for could still change dramatically.
There's one caveat to this for 2024: For the first time, HealthCare.Gov (as well as Covered California) will be automatically moving passive-renewal enrollees to lower-cost plans if they meet certain criteria (ie, the new plan has to have the same provider network, the same drug formulary, be from the same carrier and so forth...and they'll only do it if it saves the enrollee money). Even so, I'd still advise actively shopping to get the best value.
IN SHORT: SHOP AROUND, SHOP AROUND, SHOP AROUND!