Mazel Tov to the #ACA on its bar mitzvah! #ACA13 (part 3)
Note: I'm breaking this analysis into several sections:
Part 1 / Part 2 / Part 3 / Part 4 / Part 5 / Part 6 / Part 7
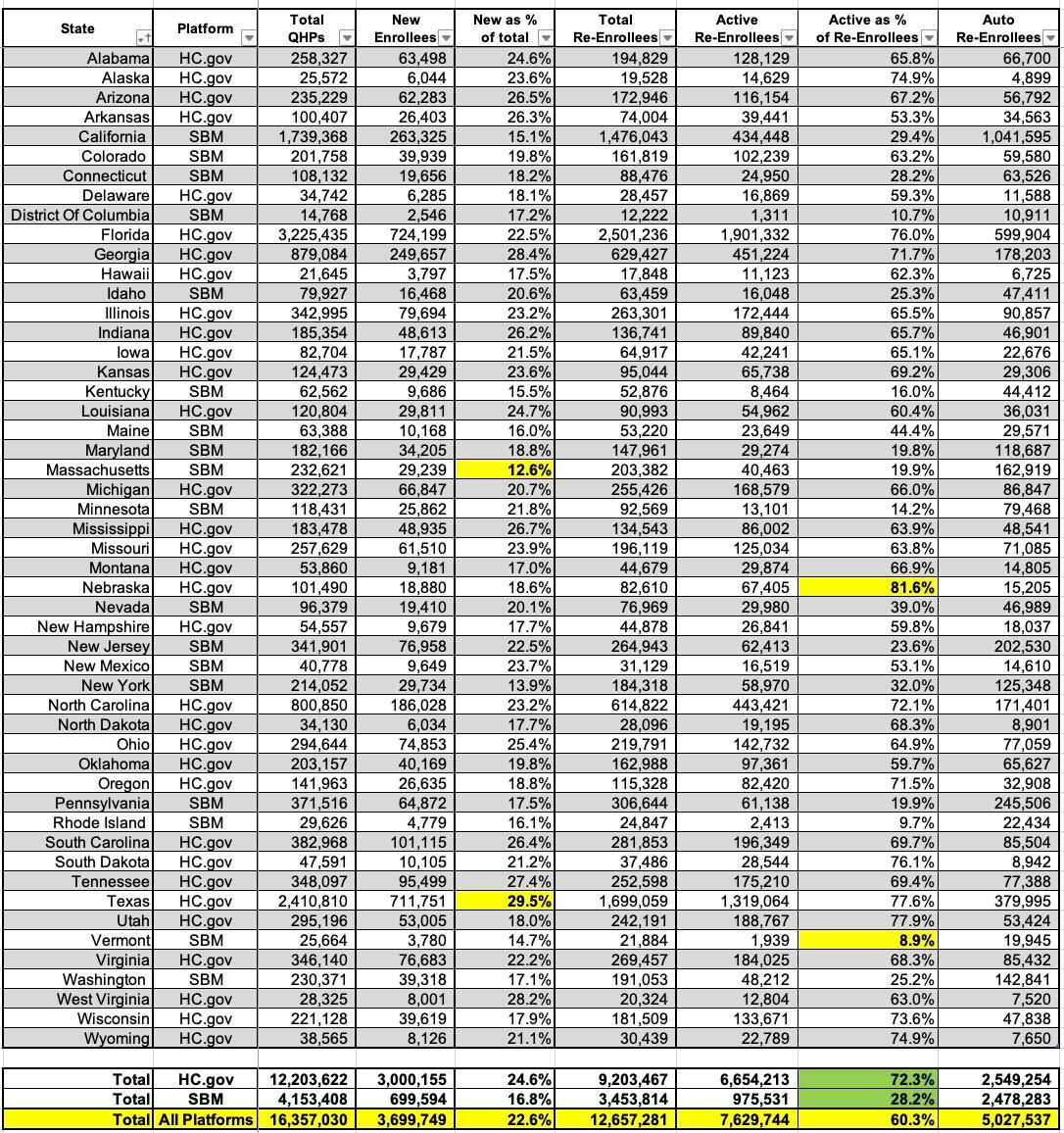
Now it's time to move on to the actual demographic breakout of the 2023 Open Enrollment Period (OEP) Qualified Health Plan (QHP) enrollees.
First up is breaking out new enrollees vs. existing enrollees who either actively re-enroll in an exchange plan for another year or who passively allow themselves to be automatically renewed into their current plan (or to be "mapped" to a similar plan if the current one is no longer available).
Nationally, around 22.6% of all exchange QHP enrollees were new enrollees this year, with the other 77.4% being current enrollees who signed up for another year. Massachusetts had the lowest percent of new enrollees out of their total enrollment at just 12.6%; this makes sense since Massachusetts has the lowest uninsured rate in the nation to begin with, at just 2.5% as of 2021. Basically, the pool of uninsured MA residents is just far smaller at this point (this is relative, of course...2.5% of ~7 million Bay Staters is still 175,000 people).
At the opposite end, nearly 30% of Texas QHP enrollees are brand new to the ACA exchange this year. Much of this is, again, likely due to a combination of them not having expanded Medicaid along with their newly-implemented Premium Alignment policy, which has the effect of dramatically increases federal subsidies for enrollees earning more than 200% of the Federal Poverty Level (FPL).
The other eyebrow-raising stat can be found a few columns over, in the "Active Re-enrollee" section. Overall, an impressive 60% of renewing enrollees actively shopped around this year, which is a good thing...but the gap between federal and state-based exchanges is stark: Only 28% of renewing SBM enrollees shopped around, while over 73% of federal exchange enrollees did. This ranges from just 9% of renewing enrollees in Vermont to a stunning 82% in Nebraska.
There's several possible reasons for this gap. While I always recommend that people shop around (even if they eventually settle on renewing their current plan anyway), in many cases they had to do so because their current carrier bailed on their state entirely. Case in point: Bright Healthcare, which announced less than a month before OEP 2023 started that they were completely pulling out of the ACA individual market in multiple states, including Arizona, Colorado, Georgia, Illinois, New Mexico, North Carolina, Oklahoma, South Carolina, Texas, Utah and Virginia.
That's over 600,000 enrollees alone who had to scramble for a new carrier...and only two of these 11 states operate their own exchanges (and even then, only ~8% of those 600K are in those states). It's a lot easier to passively renew your plan when it isn't being discontinued, after all.