10 million+ Medicaid/CHIP enrollees could lose coverage next year, but it's not necessarily all bad news...

A few weeks ago, after the Centers for Medicare & Medicaid (CMS) confirmed over 80 million Americans were enrolled in Medicaid or the CHIP program as of January 2021, I posted an analysis which looked at state Medicaid enrollment data beyond January.
While the "thru dates" vary from as early as February to as recent as June, my overall conclusion was that actual total Medicaid/CHIP enrollment as of last month has continued to grow, and now likely stands at more like 88 million. It's even conceivable that it's broken the 90 million threshold as of July.
As I noted:
Since then, the combination of sudden, massive unemployment combined with the Families First & CARES COVID Relief acts (which boost federal funding of Medicaid programs while also prohibiting states from disenrolling current Medicaid enrollees during the public health crisis) have resulted in overall Medicaid enrollment rising dramatically over the past year and a half.
What goes up usually goes back down eventually, and that's likely to be the case with Medicaid enrollment as soon as the public health crisis formally ends...whenever that may be.
Well, yesterday Ryan Levi and Dan Gorenstein of of the Tradeoffs healthcare policy podcast posted a new episode which attempts to dig into just when that might be, how many people could be kicked off of the program once that time comes and how to mitigate the fallout (I should note that they actually reference my own estimate in the program notes):
In March 2020, Congress offered states additional Medicaid funding as long as they agreed to keep everyone enrolled in the program for the duration of the federal public health emergency, regardless of their eligibility status. As of January 2021, nearly 10 million had joined Medicaid or the Children’s Health Insurance Program (CHIP) during the pandemic, pushing enrollment to a record high of more than 80 million people. (Some independent analyses put the current total higher, closer to 90 million.)
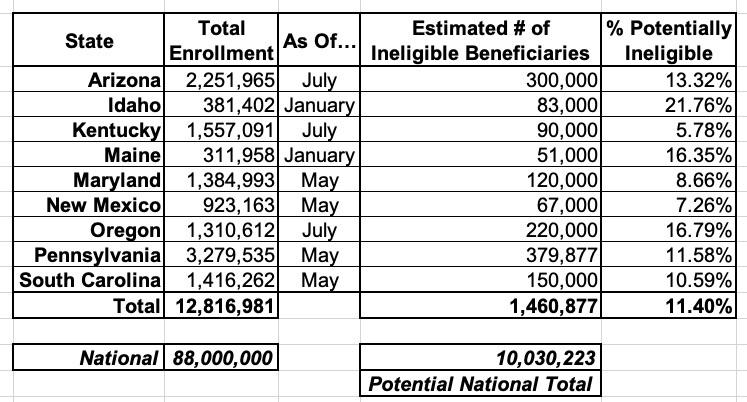
The Biden administration has indicated the public health emergency will last at least through the end of 2021. Once it expires, states will once again be required to remove ineligible people from their rolls. While no national estimates exist for how many people currently enrolled in Medicaid are technically ineligible, a Tradeoffs survey of state Medicaid offices found that just nine states expect an estimated 1,450,877 of their current beneficiaries are ineligible and would lose coverage once the health emergency ends (see table below).
This suggests that nationwide, millions are likely to lose their coverage, which is in line with expert expectations that much of Medicaid’s growth during the pandemic is a result of the continuous enrollment requirements.
I've reformatted the Tradeoffs table slightly to be alphabetical and have also taken the mid-point of the Kentucky range in order to extrapolate how many people are likely to be ruled ineligible once the emergency formally ends:
I should note that a few of the numbers above (Arizona, Kentucky and Oregon) are actually even more recent than my own:
- Arizona enrollment is 13,151 higher as of July than my May estimate
- Kentucky is 47,250 lower as of July than my June estimate
- Maryland is 19,984 lower as of May than my May estimate
- New Mexico is 3,580 lower as of May than my April estimate
- Oregon is 118,313 higher as of July than my June estimate
- Pennsylvania is 19,938 higher as of May than my April estimate
- South Carolina is 289,641 higher as of May than the official January figure via CMS
I didn't check Idaho or Maine because both of those are older than my own estimates, but for the other 7 states that's over 370,000 more enrollees as of this spring/summer than my figures indicated.
Obviously Medicaid enrollment and eligibility levels vary greatly from state to state, so I don't know how representative these 9 are, but it suggests that at least 10 million Americans could get the boot from Medicaid and/or CHIP programs sometime early next year, or over 11% of the total nationally. Some estimates put the national total as high as 15 million.
Of course, the reason why these folks would be disenrolled from the program is supposed to be because their financial or other circumstances have since improved to the point that they no longer qualify. If they're doing much better financially and no longer "need" Medicaid for their healthcare expenses, that's a good thing.
So what's the problem? Well, it's twofold: First, some states have absurdly stingy financial thresholds for traditional Medicaid enrollees in the first place. For instance, in Florida, while children are eligible for Medicaid or CHIP if the family's household income is up to 210% of the Federal Poverty Level (the program eligibility depends on income and age), their parents are only eligible up to 30% FPL. 100% FPL for a family of 4 is just $26,500/year, and Florida hasn't expanded Medicaid under the ACA, so 30% of that is just $7,950/year...or $663/month.
If that family became eligible to enroll in Medicaid last year because they only earned $660/month but by next January they've only managed to bump it up to, say, $680/month, the parents will be given the boot even though that extra $20/month doesn't exactly mean they're living large now.
The second major problem is laid out in the podcast itself, as well as by Levi on Twitter:
Finally, Trump's CMS encouraged states in Dec. 2020 to prep for the end of the PHE by checking eligibility during the pandemic and said they could use redeterminations that were up to 6 months old. A lot can change in 6 months during a pandemic.
— Ryan Levi (@ryan_levi) July 9, 2021
Biden's CMS told me that it's evaluating the 6 month rule and the rest of that Dec. 2020 guidance and will likely released updated guidance soon. Experts expect that guidance to be more "beneficiary friendly" and lean more toward giving states more time to do this work.
— Ryan Levi (@ryan_levi) July 9, 2021
...all of which sets up some logistical headaches:
HHS says PHE "will likely" last thru 2021.
Several Medicaid offices told me they take that to mean it'll end 12/31/21 — so states would lose their extra $ and have to start moving folks off rolls on Jan. 1.
"That would create a true cliff," said @AHCCCSgov director Jami Snyder.
— Ryan Levi (@ryan_levi) July 9, 2021
To do this right, Medicaid directors say they need:
- As much time as possible
- Clarity on when the PHE will end
- Congress to keep sending extra money even after the PHE ends— Ryan Levi (@ryan_levi) July 9, 2021
Of course with the #DeltaVariant now raging and a huge chunk of the population refusing to #GetVaccinated, it's conceivable that this problem will become moot for awhile longer than expected...
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.