Pennsylvania: More ugly ACA data caused by expiration of enhanced subsidies

A few minutes ago I posted a press release from Pennie (Pennsylvania's state-based ACA exchange). The release mostly focuses on the upcoming final Open Enrollment Period deadline for February coverage in the Keystone State (January 31st), but it also includes a couple of depressing (if completely predictable) stats at the end:
Costs have risen by 102% for Pennie enrollees in 2026 due to the expiration of the enhanced premium tax credits. Congress has not extended these critical savings. To date, over 70,000 Pennsylvanians have dropped coverage as a result of the higher prices – nearly 1,000 a day for most of Open Enrollment. More information can be found at pennie.com/affordability.
I did indeed visit that link, where I found the following additional details (the data provided is as of January 20th...unfortunately they don't actually list the total 2026 plan selections anywhere for some reason):
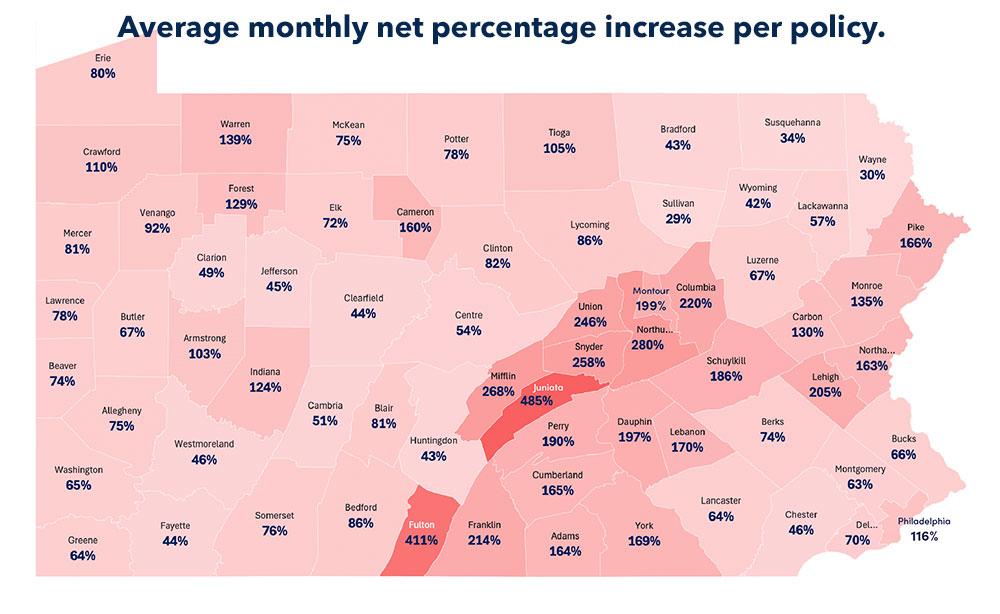
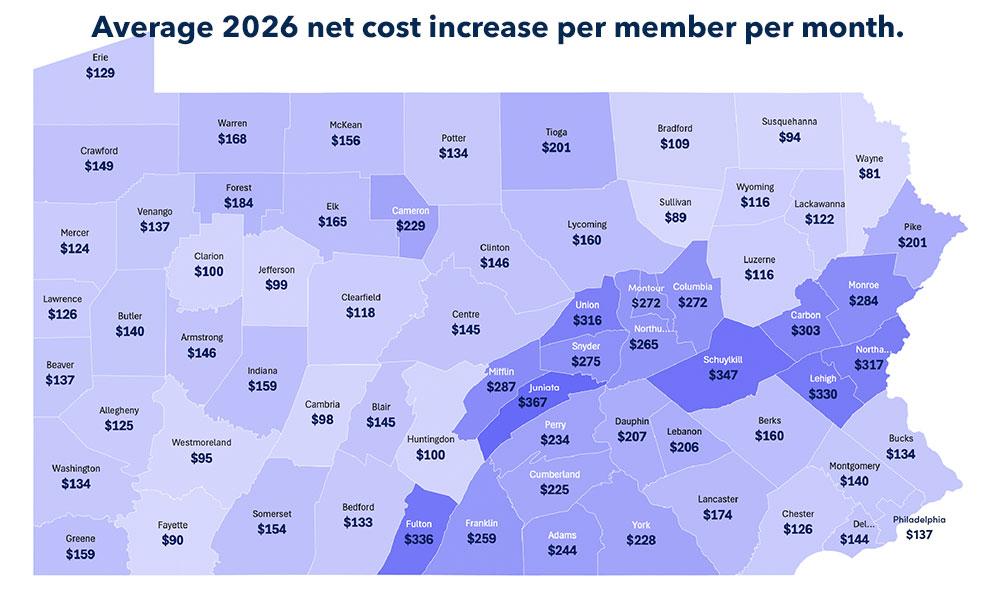
- Rural counties are experiencing a disproportionately high financial impact, as rural residents will lose more premium tax credit dollars than those in urban counties.
- Urban counties have more enrollees and are expected to have higher levels of disenrollment due to the expiration of the enhanced premium tax credits.
-
Since the start of open enrollment, Pennie has seen a 25% decrease in new enrollees from OE 2025 to OE 2026.
They don't give the hard numbers on this, but Pennsylvania had 90,472 new enrollees during OE 2025, so that's a drop of around 22,600 (more new enrollees will still come thru in the final week or so of Open Enrollment).
This means PA has around 67,800 new enrollees...but they've also had 71,816 existing enrollees drop coverage, so that's a net loss of at least 4,000 enrollees so far, or down at least 0.8% vs. last. year.
For comparison, as of 12/27, CMS had Pennsylvania ACA enrollment up around 5,900 people or up 1.3% vs. the same point last year. Once again, this blows a hole in the WSJ's recent bullshit claims regarding 2026 ACA enrollment numbers, which were based on absurdly premature data.
- 19,571 PA enrollees earning less than 150% FPL have dropped coverage, or 16.7% of the total in that income range.
This is important when looking at California, where enrollment of those below 150% FPL has increased 9% y/y thanks to the state backfilling 100% of lost federal tax credits for all enrollees earning up to 150% FPL.
There were 263,132 CA enrollees < 150% FPL last year, which suggests that if CA hadn't covered those lost subsidies, an additional ~44,000 enrollees in that income range would have dropped coverage as opposed to ~22,800 more enrolling.
-
PA enrollees ages 55-64 are terminating coverage at the highest levels among all age groups.
-
Younger, healthier PA individuals ages 26-34 are terminating coverage at the second highest levels among all age groups, which adversely impacts risk pools and drives premiums higher.
One of the graphs they provide breaks out average real world net premium hikes for 2026 enrollees at different income levels.
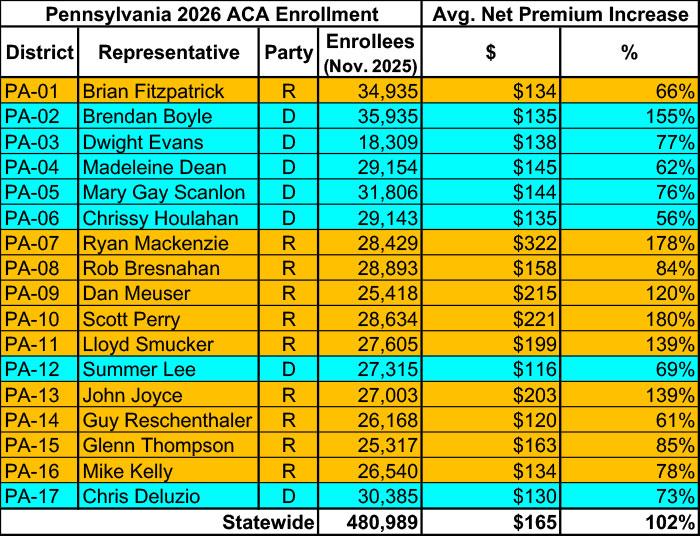
Pennie also provides a handy tool which breaks out the impact of the enhanced tax credit expiration on rate increases for all 17 PA Congressional Districts. They do include the number of effectuated enrollees as of the start of the Open Enrollment Period (that is, as of Nov. 1st, 2025):