Oh yeah...4 out of 5 Medicaid enrollees are now privately administered as well.

Earlier today I noted that according to the most recent Medicare enrollment report from the Centers for Medicare & Medicaid Services (CMS), Medicare Advantage enrollment--in which a private insurance carrier is paid by the federal government to administer Medicare benefits, and which differs in some important ways from "traditional" or "Fee for Service" Medicare--is on the verge of overtaking traditional Medicare in terms of total enrollment.
As of May 2023, 48.5% of all Medicare enrollees were covered via a Medicare Advantage plan, a percentage which has been steadily increasing over the years (it was only at 35.5% as of 2019).
While I mention this every time I post about the latest Medicare enrollment report, it's been some time since I've checked on the traditional vs. privately administered variants of Medicaid enrollees. For a long time I've been under the impression that roughly 70% of Medicaid enrollment was handled via Managed Care Organizations (MCOs):
Managed Care is a health care delivery system organized to manage cost, utilization, and quality. Medicaid managed care provides for the delivery of Medicaid health benefits and additional services through contracted arrangements between state Medicaid agencies and managed care organizations (MCOs) that accept a set per member per month (capitation) payment for these services.
By contracting with various types of MCOs to deliver Medicaid program health care services to their beneficiaries, states can reduce Medicaid program costs and better manage utilization of health services. Improvement in health plan performance, health care quality, and outcomes are key objectives of Medicaid managed care.
Some states are implementing a range of initiatives to coordinate and integrate care beyond traditional managed care. These initiatives are focused on improving care for populations with chronic and complex conditions, aligning payment incentives with performance goals, and building in accountability for high quality care.
Of course, that's the official definition/description of MCOs according to the official Medicaid.Gov website. In practice, of course, some MCOs are better than others, and there are more than a few complaints about how effectively or efficiently MCOs handle their responsibilities just as there is with Medicare Advantage.
Regardless, for better or for worse, MCOs handle most Medicaid enrollment, so I decided to take a look and see where that stands as of today.
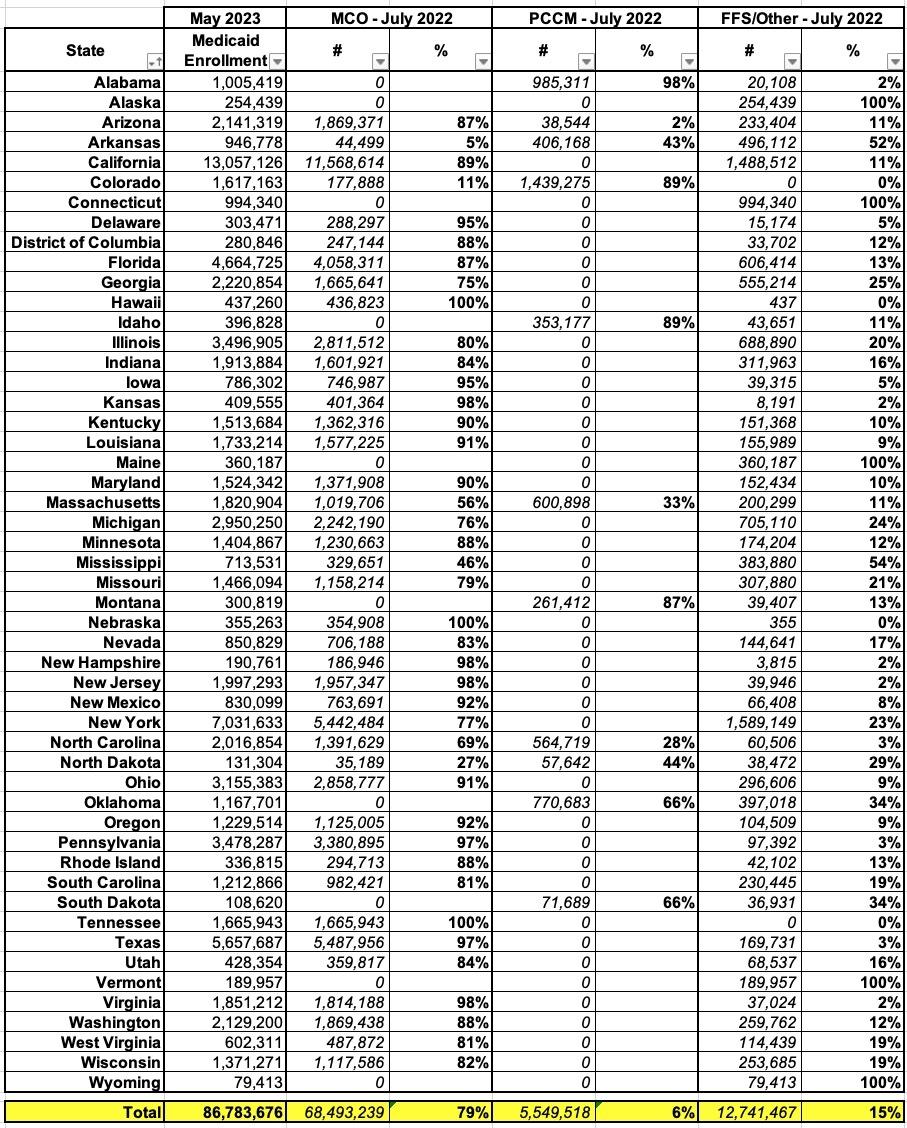
To do so, I first used this table from the Kaiser Family Foundation, which breaks out the Share of Medicaid Population Covered under Different Delivery Systems. They actually include three different delivery systems: Fee for Service (FFS), MCOs, and "PCCMs:"
PCCM refers to Primary Care Case Management. PCCM programs retain fee-for-service (FFS) reimbursements to providers, but enroll beneficiaries with a primary care provider who is paid a small monthly fee to provide case management services in addition to primary care.
Hmmm...ok, so PCCMs appear to be mostly FFM-based. Huh.
In any event, the KFF data apparently only runs through about a year ago (July 2022), but I don't imagine it's changed too much since then.
I then looked up the latest Medicaid enrollment report as of May 2023, just four months ago. This report breaks out both Medicare and CHIP (Childrens Health Insurance Program) enrollees for every state, as well as the combined totals. I don't know whether or not CHIP enrollees are handled the same way as Medicare (FFS, PCCM, MCO) in every state, so for my purposes I'm only including the ~86.8 million actual Medicaid enrollees.
Put these tables together and voila, here's where things stand:
Welp. There you have it: As of July 2022, 79% of all Medicaid enrollment was privately administered nationally.
This ranges from none at all in Alabama, Alaska, Connecticut, Idaho, Maine, Montana, Oklahoma, South Dakota, Vermont and Wyoming (although some of these use PCCM programs for a portion of their enrollees)...to as much as 100% in Hawaii, Nebraska and Tennessee.
Interestingly, there doesn't seem to be any particular pattern in terms of partisan lean or whether or not the state has expanded Medicaid under the Affordable Care Act--some red states like Alaska and Wyoming are still using 100% traditional Medicaid, while blue states like Hawaii have fully embraced MCOs, and vice versa.
Overall, however, the fact remains that nearly 80% of all Medicaid enrollees are now privately managed.
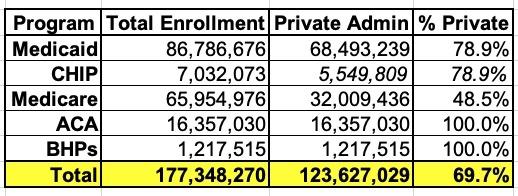
Combine that with the 48.5% of Medicare enrollees who are, and that means that between the two programs, nearly 66% are privately administered as of today.
Again, I'm not sure how the ~7.0 million CHIP enrollees are handled; assuming the FFS/MCO split is similar to Medicaid that would make it about 2/3 privately administered.
As I've said before, I am not a fan of Medicare Advantage and I have no particular love for MCOs either, but when you also include the ~16.4 million individual market ACA enrollees and the 1.2 million Basic Health Plan enrollees in Minnesota and New York, and it looks like something like this:
That's nearly 70% of all "public" healthcare coverage which is actually privately administered nationally, for good or for bad.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.