NEW: CMS confirms *effectuated* ACA enrollment *and* "How Many Have Paid?" are at all-time highs

Earlier this afternoon, the Centers for Medicare & Medicaid Services (CMS, which should really be CMMS) released a much-awaited (by healthcare wonks) Effectuated Enrollment Report for Affordable Care Act on-exchange enrollment.
While nearly 16.4 million Americans selected Qualified Health Plans (QHPs) via the federal and state ACA exchanges/marketplaces during the official 2023 Open Enrollment Period (along with an additional 1.2 million signing up for a Basic Health Plan (BHP) program in New York & Minnesota, which CMS continues to inexplicably treat as an afterthought in such reports), not all of them actually pay their first monthly premium (for January) for various reasons:
- In some cases there may be residency documentation verification issues;
- In some cases there may be technical glitches which prevented their enrollment from being effectuated;
- In some cases they may have found some other type of healthcare coverage (i.e., a job offer with healthcare benefits came through at the last minute, so instead of cancelling their enrollment they just didn't bother paying the premium & were removed from the roles)
A decade ago, during and immediately after the first, batshit insane Open Enrollment Period which ran for 6 1/2 months from October 2013 - mid-April 2014, Congressional Republicans were obsessed with the idea that vast numbers of "Obamacare" enrollees were phantoms--that is, that either the Obama Administration was flat-out making them up or that millions of people were "signing up" for exchange policies but never actually paying for it or having their policies go into effect.
This became a bit of a running joke at the time...
A hardy perennial now enjoying a revival is the “How many have PAID???” freakout. Independent ACA statistics tracker Charles Gaba has put this one under his microscope. His conclusions are that, first of all, the issue is probably exaggerated and, second, it’s way premature even to count nonpaying enrollees, because many of them won’t even receive bills for weeks yet. (We’re indebted to Gaba for the triple-question marks in our headline, as well as for resurrecting the useful term “freakout.”)
It got so out of hand that the then GOP-controlled House Energy & Commerce Committee (which was chaired at the time by Republican Representative Fred Upton from here in Michigan) actually sent out a (deeply flawed) survey to a bunch of insurance carriers demanding to know how many ACA exchange enrollees had actually paid their first premium. They then posted the results of their "survey" and attempted to make a huge stink about how, supposedly, only 67% of enrollees had done so.
I tore their survey and press release to shreds at the time by noting obvious flaws like the fact that the 67% figure assumed that all enrollees as of 4/15 were supposed to be due by 4/15 (in fact, only about 63% of the total enrollments were due by 4/15; the rest weren't due until April 30th...the same day of the press release. Of course there's also the minor detail that the survey itself was sent out on March 13th, even though, again, around 40% of enrollees for 2014 didn't even sign up until after March 15th.
When the dust settled, it turned out that somewhere around 85% or more of enrollees did indeed pay up for at least the first month, though this varied by state and carrier.
Over the years, as the federal & state exchange systems have improved and streamlined their enrollment processes and the ACA enrollment system has settled down and largely standardized itself, the percent of enrollees who make that critical first premium payment has increased, to the point that as of 2018, around 90% were doing so.
Since then, the biggest major upgrades in the ACA as a whole have been the dramatic improvement in the financial subsidy formula thanks to the American Rescue Plan and Inflation Reduction Act, as well as the implementation of the so-called "Silver Loading" pricing strategy in numerous states. Both of these have combined to offer zero premium healthcare plans to many ACA enrollees...and of course it's a lot easier to get people to pay their premium each month if that premium is nothing.
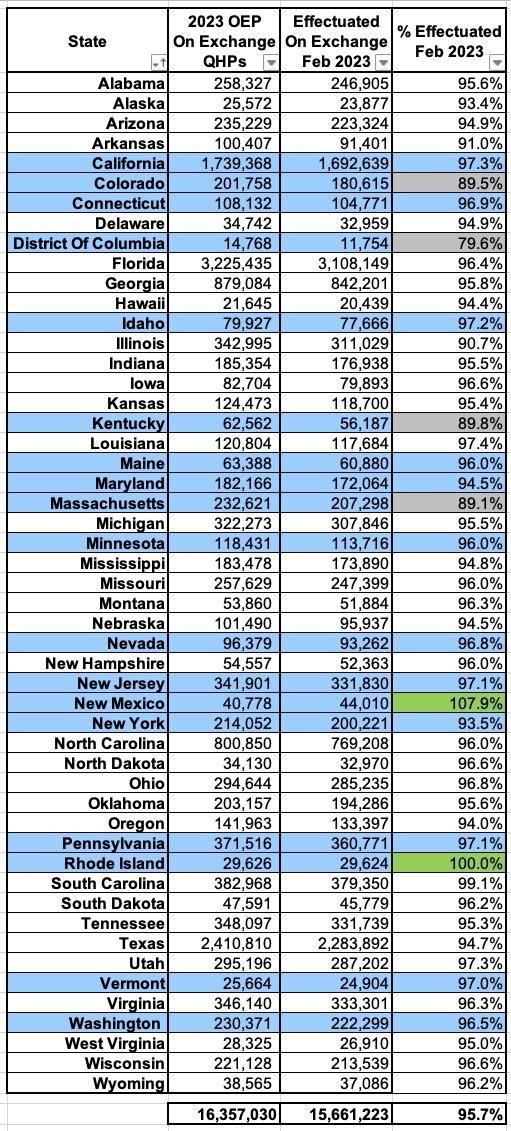
In any event, today's Effectuated Enrollment report makes it clear that the enhanced ARP/IRA subsidies + Silver Loading have indeed increased not only total enrollment, but also the effectuation percent of those enrollees:
This report provides effectuated enrollment, premium, advance payments of the premium tax credit (APTC), and cost sharing reduction (CSR) data for the Federally facilitated and State-based Marketplaces (the Marketplaces) for February 2023 and for the entire 2022 plan year, as of March 15, 2023.
Effectuated enrollment reflects the total number of people with active policies at any point within the given time period who also paid their premium, if applicable.
Key findings from this report include:
February 2023 Effectuated Enrollment, Financial Assistance, and Premiums
- Effectuated Enrollment: Effectuated enrollment through the Marketplaces for February 2023 was 15.7 million. This is a 13 percent increase from 13.8 million consumers who had effectuated coverage in February 2022. The increased coverage over this period reflects continued impacts of the APTC expansion provided by the American Rescue Plan (ARP) and the Inflation Reduction Act (IRA). This represents 96 percent of consumers who made plan selections during the 2023 Open Enrollment Period (16.4 million)
Boom: 96%.
Now, there is an important caveat to this which I'll address below, but first, here's the other above-the-fold findings:
- Financial Assistance: In February 2023, 14.3 million Marketplace enrollees, or 91 percent of total Marketplace enrollees, received APTC, a 15 percent increase from the 12.5 million enrollees who received APTC in February 2022. Additionally, CSR enrollment increased by 11 percent from 6.8 million consumers in February 2022 to 7.6 million consumers in February 2023.
APTC = Advance Premium Tax Credits. This is primarily thanks to the ARP/IRA subsidy expansion, although some of it is also thanks to Silver Loading in some states.
- Premiums: The average total monthly premium before APTC for Marketplace enrollees in February 2023 was $604.78, compared to $586.56 for February 2022. The average total premium per month paid by consumers after APTC fell by 3 percent from $127.03 in February 2022 to $123.69 in February 2023, primarily due to the expanded APTC provided by the ARP and IRA.
As noted above, the report also provides a full-year analysis of 2022 ACA exchange enrollment:
2022 Average Monthly Effectuated Enrollment, Financial Assistance, and Premiums
- Effectuated Enrollment: A monthly average of 13.5 million consumers effectuated enrollment through the Marketplaces in the 2022 plan year. This is a 15 percent increase from the average monthly effectuated enrollment of 11.7 million in the 2021 plan year.
- Financial Assistance: 90 percent of Marketplace enrollees received APTC on average each month in 2022. This represents a 2-percentage point increase from 88 percent in 2021.
- Premiums: The average total monthly premium for Marketplace enrollees in 2022 was $580.79, compared to $574.16 in 2021.
So how does 2023 compare to prior years? Well, for February Effectuations vs. OEP QHP Selections, I have the yearly data scattered throughout various blog posts, but I'm gonna borrow it from my friend & colleague Andrew Sprung:
- 2014: n/a (OEP didn't even end until mid-April)
- 2015: unknown; estimated 80-85%
- 2016: 85.4%
- 2017: 86.2%
- 2018: 89.5%
- 2019: 92.4%
- 2020: 93.5%
- 2021: 94.1%
- 2022: 95.2%
- 2023: 95.7%
Notice how the net effectuation rate has increased every year since the first Open Enrollment Period?
There's a bunch of stuff to dig into here, but this post is getting kind of long so I'll save most of it for another one. I do need to address the caveat on effectuation rates which I referenced above, however.
The reality is that every annual effectuation report put out by CMS is going to be off by a bit because of one important factor: Off-season enrollments.
Every month there are some people who drop their ACA exchange coverage for various reasons (aging into Medicare, being redetermined over to Medicaid/CHIP, getting a job with healthcare coverage, marrying someone with employer-based coverage, or simply...dying).
However, there are also some number of people who enroll in ACA exchange plans every month even after Open Enrollment has ended, via Special Enrollment Periods. SEPs are available for people who fall into similar categories to those above--if you lose your existing coverage, get divorced, move to a different state/rating area, get out of prison, etc. you have 60 days to enroll. There are other SEPs as well, especially for those who earn less than 150% of the Federal Poverty Level and so forth.
In other words, if 500,000 people sign up for ACA coverage in a given state as of the OEP deadline of January 15th, it's conceivable that, say, 10% (50,000) may not pay their January premiums (and are thus never effectuated)...but that another 30,000 sign up and pay via SEPs between 1/15 and 1/31, which would result in a net February effectuation rate of 96%.
That's an exaggerated example for the most part, but not necessarily--in fact, if you check the February effectuation numbers against the number of OEP enrollments in the official CMS report from earlier this year, you can see that in New Mexico, the February number is higher than the OEP number...nearly 8% higher, in fact!
Now, New Mexico's exchange enrollment data got a bit screwed up last year due to their transition from a federal to a state-based exchange the year before, so this may be a lingering part of that...but also note that Rhode Island's net effectuation rate as of February 2023 is 100%...that is, had nearly the exact same number of effectuated enrollees in February as signed up during OEP. In fact, they had 2 more people.
At the opposite end of the spectrum, there are several states where net February effectuations were down more than 10%: In Colorado, DC, Kentucky and Massachusetts. The largest drop-off is DC, where only 80% of those who signed up during Open Enrollment were actually effectuated as of February.
There doesn't seem to be any particular pattern connected to partisan lean, urban vs. rural, etc...the only consistent factor is that all four utilize state-based exchanges...oh, and all four have expanded Medicaid. Not sure if I can draw any conclusions from either of those, however.
Anyway, as I said, I'll dig into the Effectuation report more deeply in another post...
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.