How much more will ~39,000 WYOMING residents pay if the improved #ACA subsidies expire? (updated)

Originally posted 2/2/25
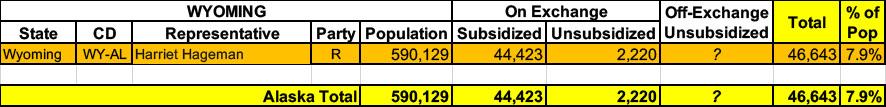
Wyoming has ~46,000 residents enrolled in ACA exchange plans, 95% of whom are currently subsidized. They also have an unknown number of off-exchange enrollees (likely only a few thousand at most). Combined, that's around 8% of their total population.
(Note, however, that the official actuarial rate filings for the 3 carriers offering coverage in the Wyoming individual market only report a combined total of around 39,000 enrollees as of spring 2025, or 6.6% of the total population).
In early 2021, Congressional Democrats & President Biden passed the American Rescue Plan Act (ARPA), which dramatically expanded & enhanced the original premium subsidy formula of the Affordable Care Act, finally bringing the financial aid sliding income scale up to the level it should have been in the first place over a decade earlier. They then extended the subsidy upgrade out by another 3 years via the Inflation Reduction Act.
In addition to beefing up the subsidies along the entire 100 - 400% Federal Poverty Level (FPL) income scale, the upgrade eliminated the much-maligned "Subsidy Cliff" at 400% FPL, wherein a household earning even $1 more than that had all premium subsidies cut off immediately, requiring middle-class families to pay full price for individual market health insurance policies.
Unfortunately, the improved subsidies are currently scheduled to end effective December 31, 2025. Needless to say, with Republicans holding a trifecta, it's highly unlikely that the IRA's enhanced subsidies are going to be be extended further. They had the opportunity to do so as part of H.R. 1 (the so-called “Big Beautiful Bill”), but chose not to.
It gets even worse:
In addition, the so-called “Affordability & Integrity Rule” put into place by RFK Jr., & Dr. Oz at the Centers for Medicare & Medicaid Services (CMS) is causing 2026 subsidies to be even less generous and gross premiums to increase even more.
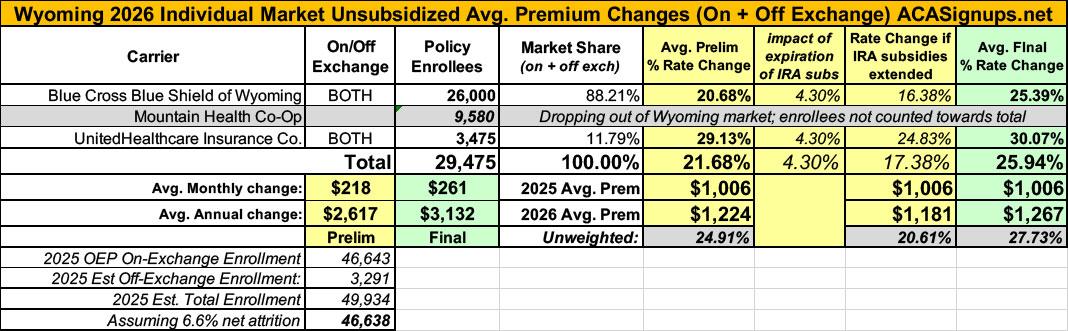
In Wyoming specifically, all of this will result in average gross premiums hikes of 25.9%.
I decided to run the numbers myself to get an idea of just how much the combination of expiring IRA subsidies and the CMS "Affordability/Integrity Rule" will cause net premiums to increase starting in January 2026.
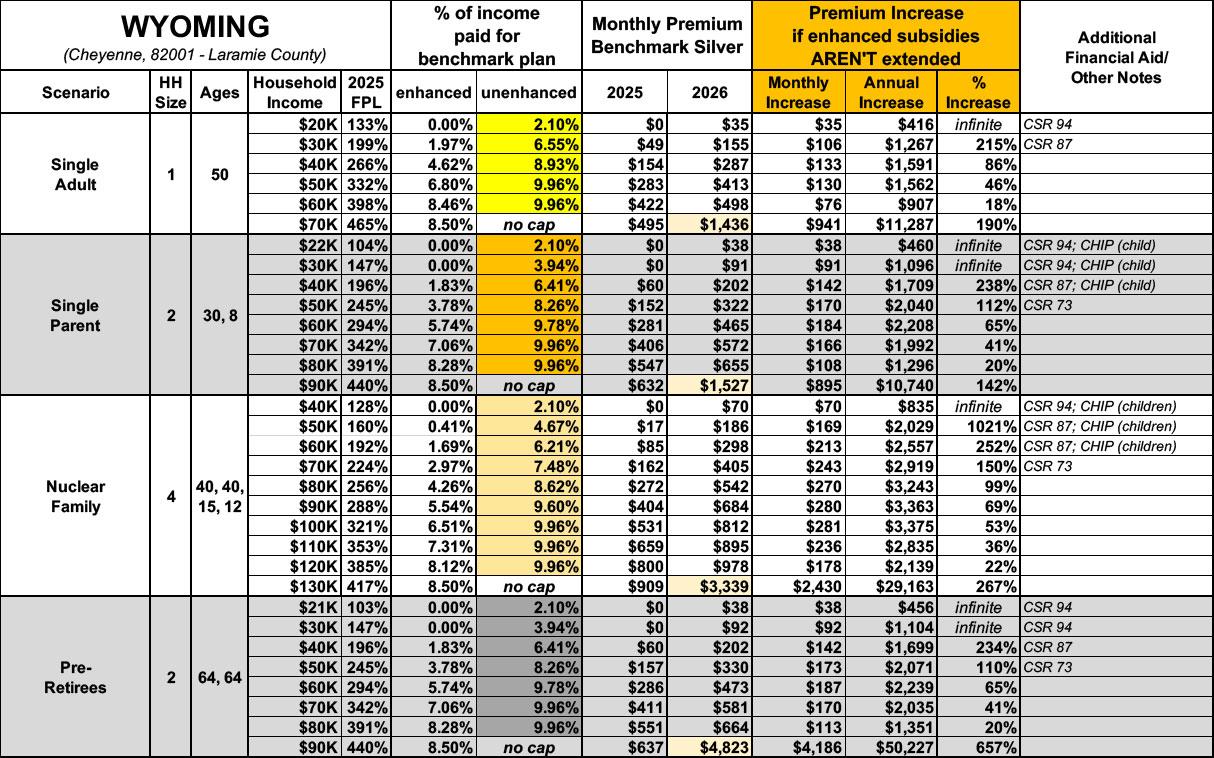
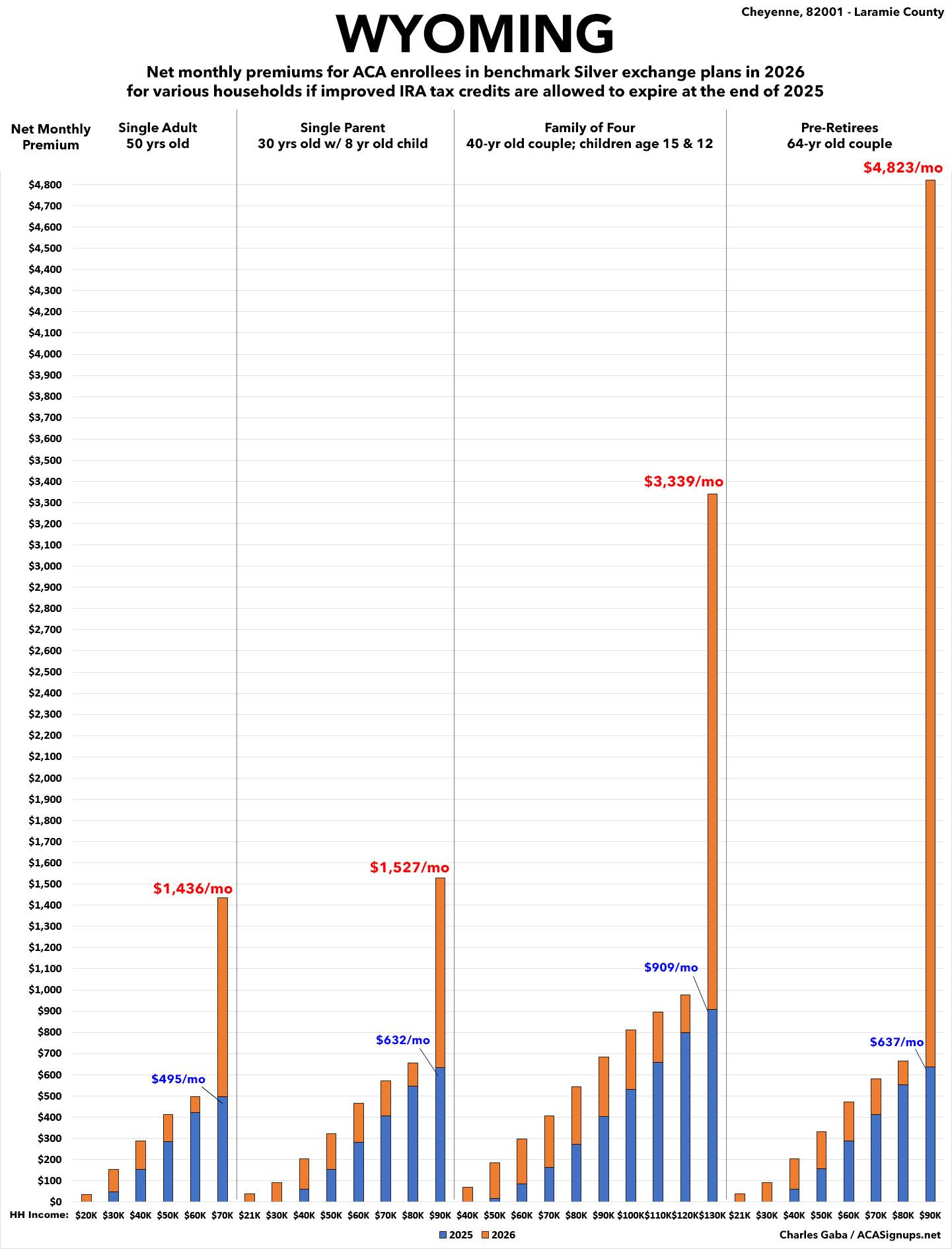
I'm using four household scenarios, at several different income levels for each:
- a 50-yr old single adult earning between $20K - $70K/year
- a 30-yr old single parent w/an 8-yr old child, earning between $20K - $90K/year
- a 40-yr old couple w/2 children age 15 & 12, earning between $40K - $130K/year
- a 64-yr old couple earning between $20K - $90K/year
There's several caveats involved here.
-
The average Benchmark Silver ACA premiums are based on 2026 levels.
-
Benchmark Silver premiums vary widely depending on where you live & other factors. For Wyoming I'm using Cheyenne.
-
In some states, children under 19 are eligible for CHIP or Children's Medicaid at a significantly higher household income level. This can cause a sudden jump in full-price premiums as the household income moves over that eligibility threshold.
-
These analyses assume that the enrollees choose the benchmark Silver plan, and that the benchmark plan remains the same both years (the actual benchmark plan often changes from one year to the next).
-
It's important to keep in mind that Wyoming is one of the 10 states which still hasn't expanded Medicaid under the ACA.
-
NEW: The original version of this analysis included a 4.3% increase in the unsubsidized benchmark plan premium based on a projection by the Congressional Budget Office. However, that was a national average projection which didn’t take into account other factors like increased utilization, medical inflation and so on. This updated version assumes the actual 2026 Wyoming rate filings.
-
NEW: The original version of this analysis assumed that the Applicable Percentage Table would revert back to the pre-2021 levels. However, the Trump Administration recently modified the formula used to calculate this which means that ACA subsidies will be even less generous starting in 2026.
With all that understood, let's take a look:
- A single 50-yr old earning just $20,000/yr would go from not having to pay anything in premiums to having to pay $35/month (technically an infinite increase). Similarly, a single parent earning just $30,000/yr would go from $0/mo to $91/mo in premiums, and a family of four earning $40,000/yr would go from $0/mo to $70/mo.
- A single 50-yr old earning $40,000/yr would see his premiums jump from $154/month to $287/month...nearly DOUBLE.
- A single parent earning $50,000/year would go from paying $152/month to $322/month...over twice as much.
- A family of four earning $70,000/year would see their premiums jump from $162/month to $405/month...2.5x as much.
- A 64-yr old couple earning $90,000/yr would go from paying $637/mo to a jaw-dropping $4,823/mo...OVER 7.5x AS MUCH FOR THE SAME POLICY. That'd be over $50,000/YR IN PREMIUMS ALONE, or 55% OF THEIR GROSS INCOME.