California: @CoveredCA announces 158K shifted from Medicaid to #ACA exchange plans thru June; up to 82% of Unwinding population have some form of coverage

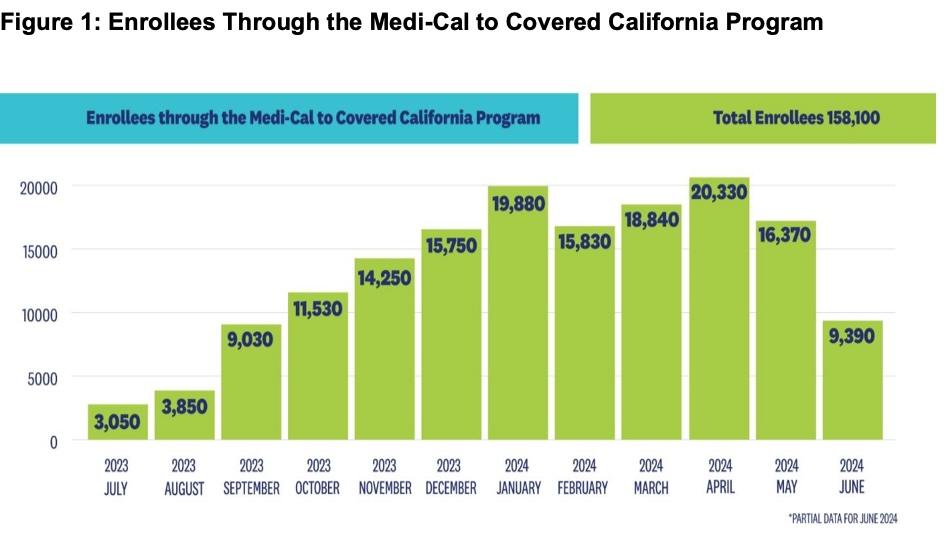
Covered California announced today that more than 158,000 Californians remained covered through the Medi-Cal to Covered California enrollment program over the past year.
Beginning in April 2023, following the end of the federal continuous coverage requirement put in place during the COVID-19 pandemic, Medi-Cal resumed its renewal process by redetermining eligibility for over 15 million of its members. In May 2023, Covered California and the Department of Health Care Services (DHCS), which administers California’s Medi-Cal program, launched the Medi-Cal to Covered California enrollment program.
Under the program, Covered California automatically enrolls individuals in one of its low-cost health plans when they lose Medi-Cal coverage and gain eligibility for financial help through Covered California. Through early June of 2024, the program has helped 158,100 Californians remain insured.
Hmmm...this is great news, but the bar graph seems to be completely at odds with the data provided by CMS which puts California's Medicaid/CHIP > Exchange QHP enrollment at 146,655 through February.
The June number being 158,100 seems reasonable (7.8% higher than CMS's February total), but the graph above claims that only 93,170 had been transferred over from Medi-Cal to CoveredCA policies. I'm also not sure I understand the significance of the different-colored horizontal bars above the vertical ones.
Assuming the 7.8% increase is representative, that would mean around 4.8 million people have been shifted from Medicaid/CHIP to exchange QHPs nationally.
“Through our partnership with DHCS, we have been able to help nearly 160,000 Californians seamlessly transition from Medi-Cal to Covered California and avoid gaps in coverage,” said Covered California Executive Director Jessica Altman. “We are proud of these results so far, and the Medi-Cal to Covered California program is now a mainstay in our effort to keep Californians covered with comprehensive, affordable health insurance.”
CoveredCA's press release also addresses the other elephant in the Medicaid Unwinding room: What about the rest of those who've had their Medicaid/CHIP coverage terminated over the past year or so? With 23 million people having been "unwound" as of a few days ago, the current healthcare coverage status of perhaps 72% of them is unknown...but in California, at least, it sounds like it's not nearly as bad as it sounds:
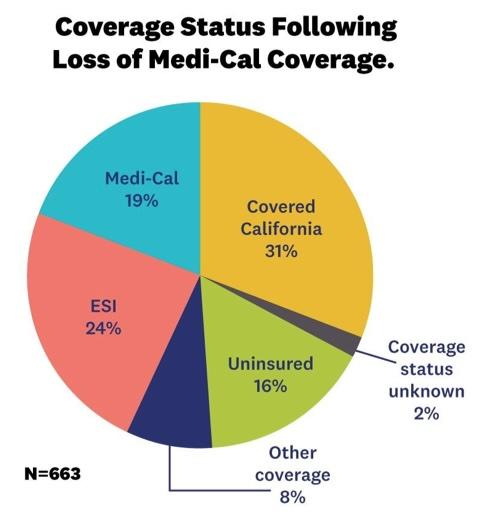
Early Survey Indicates That Most Californians Who Gain Eligibility for Covered California After Medi-Cal Retain Some Form of Health Coverage
Many people who undergo the Medi-Cal renewal process may already have acquired another source of coverage — such as a through a new job — and are no longer seeking insurance, but those who are without another source of coverage can turn to Covered California.
According to a pulse survey conducted last fall on behalf of Covered California by NORC and Slosar Research, among the first month’s cohort of consumers automatically enrolled with Covered California following the loss of Medi-Cal eligibility, 82 percent report having coverage at the end of their special-enrollment period. That figure includes 31 percent reporting enrollment through Covered California, 24 percent with employer-sponsored insurance and 19 percent returning to Medi-Cal.
While this 14-month redetermination period is ending, Medi-Cal’s normal redetermination process will continue, as will the Medi-Cal to Covered California program. Californians who are determined to no longer be eligible for Medi-Cal but who qualify for financial help through Covered California will receive information in the mail on their new Covered California plan. For eligible transitioning consumers, Covered California will automatically select a plan for the consumer that provides the most financial help.
Consumers will need to take action and confirm their Covered California plan selection and pay their first month’s premium, if one is required, in order for their coverage to take effect. Covered California urges Medi-Cal members to check their mail and respond quickly by either confirming their new plan, changing their plan or opting out of coverage.
“If you have lost your Medi-Cal coverage, time has not run out to sign up for Covered California,” said California’s Secretary of Health and Human Services and Covered California Board Chair Dr. Mark Ghaly. “California is working to keep you enrolled in affordable and high-quality health insurance to ensure you have continuity in access to health care services.”
Qualifying Californians Can Still Enroll
Covered California also reminds other Californians that they can sign up for quality health insurance through Covered California’s special-enrollment period if they experience a qualifying life event. Some of the most common reasons that someone would be eligible for special enrollment would be losing health coverage, getting married, having a baby, permanently moving to California or moving within California.
A full list of qualifying life events can be found here.
Signing Up for Coverage Is Easy
Consumers can learn more about their options by visiting CoveredCA.com, where they can easily find out if they qualify for financial help and see the coverage options in their area. Those interested in learning more about their coverage options can also:
- Get free and confidential assistance over the phone, in a variety of languages, from one of more than 14,000 certified agents and community-based organizations throughout the state that provide free, confidential help.
- Have a certified enroller call them and help them for free.
- Call Covered California at (800) 300-1506.