ASPE report digs deeper into the record 31 million Americans covered by the #ACA right now

Moments ago I posted the news that the HHS Dept. (via the Centers for Medicare & Medicaid) has confirmed what I wrote about nearly a month ago: Enrollment in ACA healthcare policies are at an all-time high, with over 31 million Americans currently covered by either ACA exchange plans, ACA Medicaid expansion or ACA Basic Health Plan coverage.
This news is based on a formal report issued by the Assistant Secretary for Planning & Evaluation (ASPE). Let's take a closer look!
Health Coverage Under the Affordable Care Act: Enrollment Trends and State Estimates
Based on enrollment data from late 2020 and early 2021, approximately 31 million people were enrolled in Marketplace or Medicaid expansion coverage related to provisions of the Affordable Care Act (ACA), the highest total on record.
KEY POINTS
- The Affordable Care Act (ACA) created new pathways to coverage via health insurance Marketplaces and Medicaid expansion in participating states, which both took effect beginning in 2014.
- As of the most recently available administrative data, 11.3 million consumers were enrolled in Marketplace plans as of February 2021, and 14.8 million people were newly enrolled in Medicaid via the ACA’s expansion of eligibility to adults as of December 2020. In addition, 1 million individuals were enrolled in the ACA’s Basic Health Program option, and nearly 4 million previously-eligible adults gained coverage under the Medicaid expansion due to enhanced outreach, streamlined applications, and increased federal funding under the ACA.
- Across these coverage groups, 31 million Americans were enrolled in coverage related to the ACA, representing the highest total on record.
- In addition, the ACA also enables young adults to stay on their parents plans until age 26, and more than 1 million new consumers have signed up for Marketplace plans during the 2021 Special Enrollment Period since February 15, 2021.
- All 50 states and the District of Columbia have experienced substantial reductions in the uninsured rate since 2013, the last year before full implementation of the ACA.
Again, it's important to note that the 18.8 million Medicaid expansion enrollee figure (14.8 million + 4.0 million) only run through December; as I've noted in several state-level analyses, Medicaid expansion has continued to grow in many states since December. It could be as high as 16 million today, though that's unknown for now (and it's probably started to drop off a bit as the economy improves and people go back to work).
METHODS
For both Marketplace and Medicaid expansion enrollment, we present the most recent administrative data with state-by-state totals from the Centers for Medicare & Medicaid Services (CMS), as well as historical national totals for the years 2014-2020.
Current Marketplace enrollment estimates are for February 2021 coverage and reflect effectuated enrollment counts calculated using the number of individuals with an active policy at any point during that month who had paid their first month’s premium, if applicable. Effectuated enrollment totals are included from both States with Marketplaces using the HealthCare.gov platform and those with State-based Marketplaces.
Medicaid enrollment estimates are state-reported counts of unduplicated individuals enrolled in the state’s Medicaid program through the Medicaid Budget and Expenditure System (MBES). The most recent Medicaid enrollment data are from December 2020.
For states that have expanded Medicaid, the enrollment data provide specific counts for the number of individuals enrolled in the new expansion adult eligibility group, referred to as the “adult group,” with separate totals for those who became newly eligible under the ACA expansion, as well as those who would have been eligible for coverage prior to the ACA but are now part of the adult group. State Medicaid expenditure reports are generally submitted to CMS within 30 days following the end of each quarter. Some states, however, submit their expenditure reports later; accordingly, these results should be considered preliminary.
Minnesota and New York have also implemented the Basic Health Program (BHP) option under the ACA to cover individuals with incomes between 138-200% FPL. We report annual average BHP enrollment, as reported to CMS by the states.
Estimates on the uninsured come from the American Community Survey (ACS), the largest national survey of households. The Census Bureau surveys almost 300,000 households each month for the ACS and collects health insurance and demographic data, along with other types of information. Uninsured rates for the full state population of all ages come from the ACS’s public data tables for 2013 and 2019 (the most current year of ACS data available), which we used to compare state-by-state changes in uninsured rates since the implementation of the ACA.
RESULTS
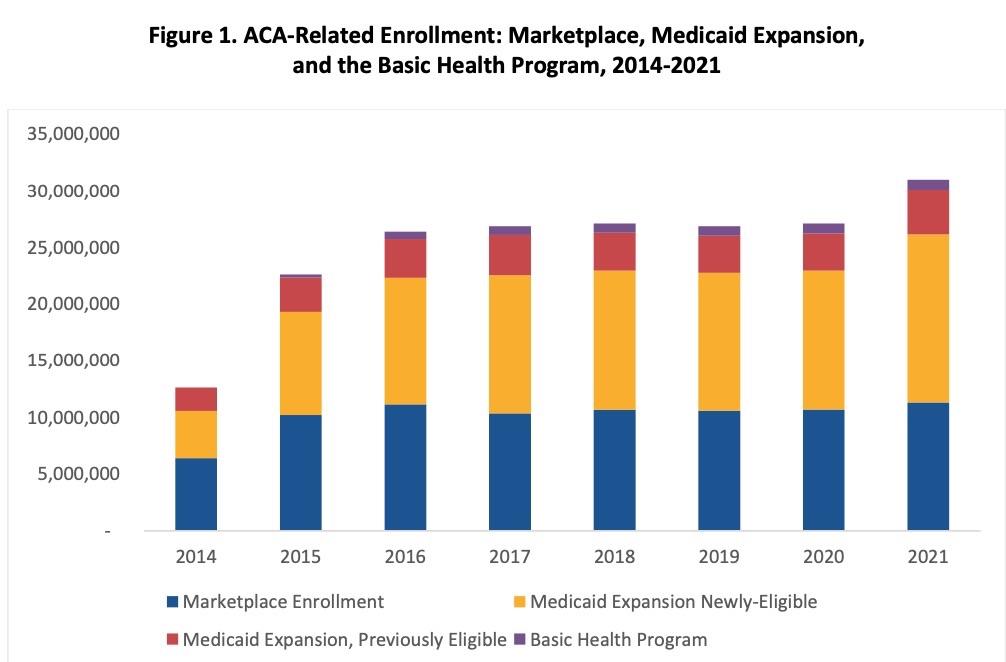
Table 1 and Figure 1 present national ACA-related enrollment for 2014-2021. As of February 2021, 11.3 million consumers had enrolled and effectuated health insurance coverage through the Marketplaces. This estimate does not include individuals who have signed up for coverage during the COVID Special Enrollment Period (SEP) for HealthCare.gov that began on February 15, 2021, and runs through August 15, 2021. Since the SEP began and new outreach funds were also made available, over 1 million additional consumers have signed up for a health plan through HealthCare.gov. This total does not include any impact from expanded SEP opportunities offered by the 15 state-based Marketplaces in 2021.
At the close of 2020, an estimated 14.8 million newly-eligible adults were enrolled in Medicaid coverage through the adult group created by the ACA expansion, as shown in Table 1. An additional estimated 3.9 million people were enrolled in the Medicaid expansion adult group under the ACA who would have been eligible for Medicaid before the ACA. The ACA, however, simplified Medicaid enrollment for these individuals and made permanent under federal law some state-specific coverage expansions that pre-dated the ACA (e.g., coverage under a section 1115 demonstration project). To date, 37 states and the District of Columbia have adopted the ACA Medicaid expansion of coverage to adults.
Two states – Minnesota and New York – have also implemented the Basic Health Program (BHP) option under the ACA, with enrollment totaling approximately 1.0 million in early 2021.
Taken together, these results indicate that overall enrollment in Marketplace coverage, Medicaid expansion, and the Basic Health Program for 2021 was approximately 31 million people, the highest enrollment total since the ACA was enacted.
And there it is:
- 11.3 million effectuated exchange enrollees
- 14.8 million newly-eligible Medicaid enrollees
- 3.9 million previously-eligible/streamlined Medicaid enrollees
- 1.0 million BHP enrollees
- 31.0 million total
And again, this does NOT include:
- At least 1.0 million SEP enrollees via HC.gov
- (This is probably more like 1.2 million as of today*)
- Likely a good 400K - 600K SEP enrollees via the state-based exchanges
- However many additional Medicaid expansion enrollees have signed up since December
*it's even possible that President Biden let this number slip in the video released by the White House a little while ago...he makes a reference to "1.2 million people signing up on top of the 30 million" which may be a preview of the next CMS SEP enrollment report through the end of May...or it may not be:
If you include all of those, total ACA enrollment could be as high as 33.5 million people...or exactly 10% of the entire U.S. population.
UPDATE: D'oh!! I completely forgot OFF-exchange ACA enrollments as well! These were pegged at 4.1 million by CMS back in 2016, and while they've dropped significantly since that time (some people moved to on-exchange plans already counted above; some moved to other types of coverage), there's still at least 1.5 million people enrolled in unsubsidized ACA-compliant policies directly via their insurance carrier. These policies are still ACA-created as they include all the patient protections of on-exchange plans.
Throw them into the mix and the grand total could potentially be as high as 35 million Americans.
Notes:
* Marketplace effectuated enrollment figures for 2014 and 2015 are as of 12/31/2014 and 3/31/2015 respectively, versus February coverage as of 3/15 for 2016-2021. Marketplace enrollment data for 2014-2015 are lower quality due to the manual payment processing system in place for those years. 2014 and 2015 Marketplace enrollment figures are published here. February 2016-2021 data are from the CCIIO Enrollment Payment System and beginning in 2017 have been published in the Effectuated Enrollment Snapshot for the respective year.
# Medicaid enrollment data, 2014-2020, are from the February monthly enrollment (ever enrolled during the month) for the expansion adult eligibility group, as reported by states through the Medicaid Budget and Expenditure System (MBES). 2021 Medicaid enrollment data are from December 2020 monthly enrollment, as this is the most recent available monthly enrollment count from MBES. Published reports and detailed data information for Medicaid enrollment data, including caveats, can be found here.
**BHP programs did not start until 2015. BHP enrollment data are based on average monthly (for Minnesota) or quarterly (for New York) projected enrollment submitted by the states to CMS in advance of the applicable quarter and are rounded to the nearest thousand. BHP enrollment data for 2021 is through May 2021.
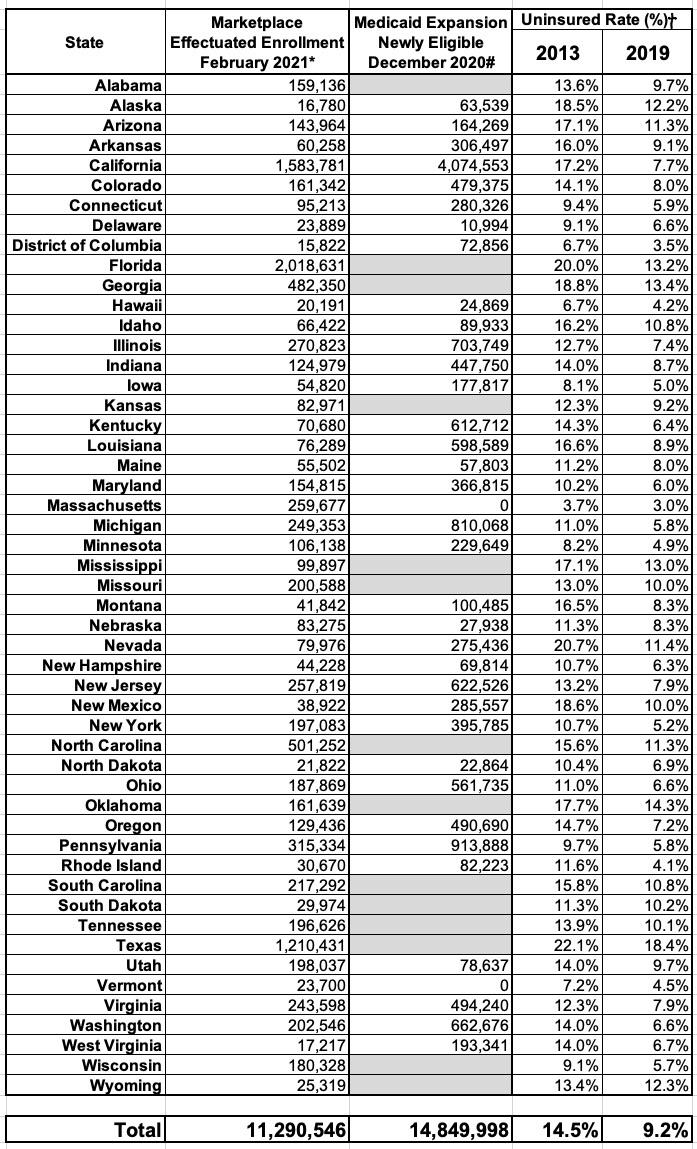
Table 2 presents enrollment estimates by state for Marketplace and Medicaid coverage, plus uninsured rates before and after the ACA. Figure 2 illustrates the percentage change in the uninsured rate from 2013-2019 for each state. Nationally, the uninsured rate has decreased 5.3 percentage points (from 14.5% to 9.2%) since the ACA coverage provisions were implemented in 2014.
All states experienced reductions in their uninsured rates, with 7 states – CA, KY, NY, OR, RI, WA, WV, all of which expanded Medicaid – reducing their uninsured rate by at least half. The uninsured rate in 2019 varied widely across the country. Massachusetts had the lowest uninsured rate at 3.0% and experienced one of the smaller relative reductions under the ACA because it had already implemented large coverage expansions prior to 2014. Texas had the highest uninsured rate at 18.4%. State decisions regarding the ACA Medicaid expansion are a main driver of this variability. The Census Bureau’s gold-standard estimates of the uninsured population, which come from the ACS, are not yet available for 2020.
The ACA is a wide-ranging law, and these estimates are a conservative estimate of the law’s impact on health insurance coverage for several reasons. First, the total does not include the impact of the COVID Special Enrollment Period in 2021. Second, the total does not include the provision of the ACA that took effect in 2010 allowing young adults to remain on their parents’ plans until age 26, which previous research estimated led to more than 2 million young adults gaining insurance.
Finally, the streamlining of Medicaid applications, enhanced outreach, and expanded eligibility led to increased enrollment even among children and parents who were eligible for Medicaid through traditional pre-expansion pathways, a phenomenon referred to as the “welcome mat” effect. Thus, 31 million likely underestimates the total effect of the ACA on coverage.
- 1 Minnesota has also created a Basic Health Program (BHP) under the ACA, which had 104,125 enrollees as of April-May 2021.
- 2 New York has also created a BHP under the ACA, which had 898,891 enrollees as of April-May 2021.
- * Marketplace Data: Effectuated enrollment, which is a count of individuals with an active policy at any point in the month of February 2021, who had paid their first month’s premium, if applicable, as of March 15, 2021.
- # Medicaid Data: Monthly enrollment of newly eligible population as reported in December 2020 on the CMS-64, updated in May 2021. Awaiting state reporting, enrollment reasonableness review is in progress. Enrollment only applicable for states that have expanded their Medicaid programs to Adults with incomes up to 138% FPL (the “adult group”). For the states that have not expanded Medicaid their enrollment is noted as “N/A.” Massachusetts and Vermont already offered subsidized coverage to those with incomes below 138% FPL, so they are listed as having 0 newly-eligible adults, even though they have implemented the ACA’s Medicaid expansion.
- Uninsured Rates: American Community Survey, “Health Insurance Coverage Status and Type of Coverage by State and Age for All People”, 2013-2019
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.