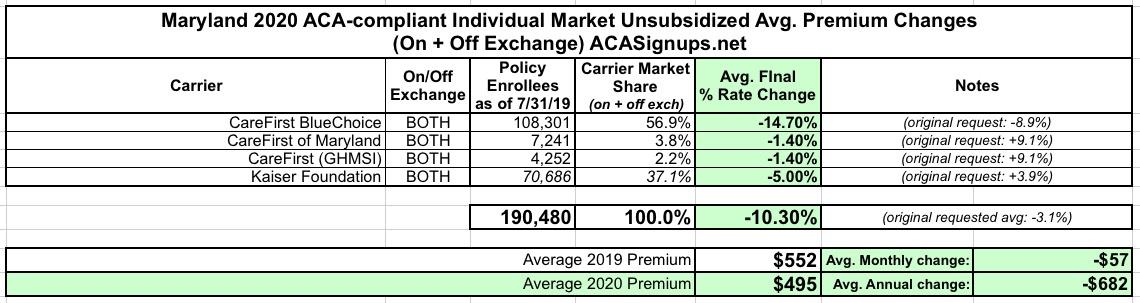
Maryland: *Approved* 2020 ACA Exchange Premium Rate Changes: 10.3% reduction
Back in May, Maryland was the very first state to publicly release their preliminary 2020 individual and small group market rate change requests. For 2019, thanks to several laws passed by the state legislature and signed by Gov. Hogan, including a robust ACA Section 1332 reinsurance waiver program, instead of increasing by another 30%, premiums dropped by 13.4% this year.
For 2020, the preliminary rates looked pretty good: Average rates were expected to drop by around 3% or so.
Well, today the Maryland Insurance Department announced the approved rates for 2020...and it's even better than that:
Hogan Administration Announces Second Consecutive Decrease in Health Insurance Premiums
Maryland Insurance Administration Announces 10.3% Average Decrease for Individual Market in 2020; Consumers Benefit from Year Two of State Reinsurance Program
ANNAPOLIS, MD – Governor Larry Hogan today announced that the Maryland Insurance Administration (MIA) has approved an average 10.3% premium rate decrease for individual health insurance plans with an effective date of January 1, 2020. This means that, for the second consecutive year, all individual insurance rates in Maryland will see important decreases.
The new rates reflect the impact of the State Reinsurance Program, which has helped to lower rates and stabilize the individual health insurance market after years of major premium increases. Coupled with last year’s decrease of 13.2%, the two-year cumulative impact is a rate decrease of more than 22% versus 2018 premiums.
“By addressing this crisis head-on, we have gone from an individual market on the brink of collapse to two straight years of lower premiums for Marylanders,” said Governor Hogan. “Last year, after we refused to accept Washington’s failure to act, we came together to deliver lower rates for the first time in more than a decade. Our innovative program to make healthcare more affordable for Marylanders serves as a model for the rest of the nation.”
In 2018, facing predicted health insurance rate increases of up to 50%, the Hogan administration worked in bipartisan fashion with legislative leaders to develop landmark legislation establishing a state reinsurance program. The legislation directed the Maryland Health Benefit Exchange to submit a State Innovation Waiver under Section 1332 of the Affordable Care Act (ACA) to the U.S. Secretaries of Health, Human Services, and Treasury to establish the program. The legislation combined with this waiver set up a reinsurance pool to provide funding for catastrophic claims for policyholders in the individual market.
“After years of devastating rate increases, it is certainly gratifying to see our individual market begin to stabilize,” said Maryland Insurance Commissioner Al Redmer, Jr. “The approved rates have improved over what was originally proposed, due to the hard work of our Chief Actuary and his team, as well as the collaborative work of the insurer's actuarial teams. We are hopeful that those Marylanders that continue to go uninsured will investigate the benefits and federal subsidies that may be available to them.”
I need to point out one person who doesn't get formal credit from the Hogan Administration, and rightly so: CMS Administrator Seema Verma. Yes, she deserves acknowledgement for approving the waiver, but that's pretty much it--the actual work itself was done by state legislators, Gov. Hogan, the Maryland Insurance Dept. and so forth. Verma has had the chutzpah to try and lay claim to the various reinsurance waivers even though they're already part of the very law she's trying to have eliminated, and it's good to see that a Republican Governor isn't letting her steal credit for it.
To assist the administration in making its rate decision, MIA actuaries reviewed the data, methodologies, and assumptions companies used to develop their proposed premium rates. The MIA also considered public comments, along with other relevant factors, in determining whether to approve, modify or deny requested rates.
There's two other laws which also should've had an impact, although these are harder to pinpoint:
- The crackdown by the state on #ShortAssPlans in 2018 (which had a small but positive effect for 2019 rates), and...
- The recently-passed "Easy Enrollment" law which goes into effect next year, which should help boost both Medicaid expansion and subsidized exchange enrollment.
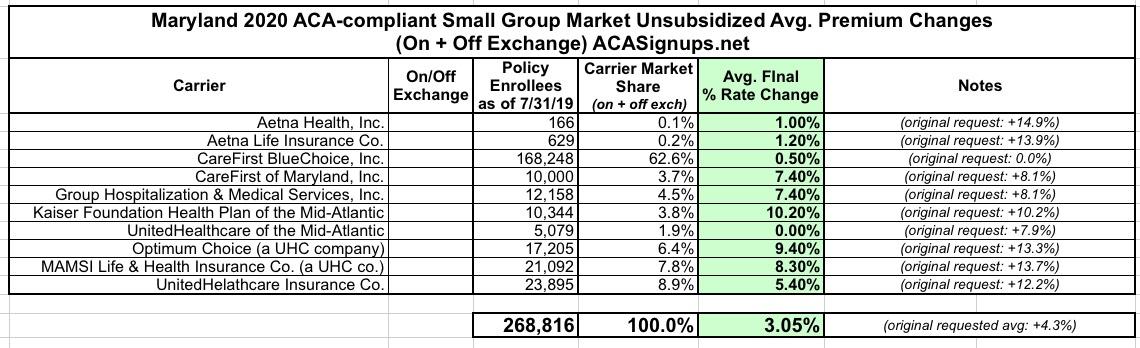
Here's the final, approved rate changes by carrier in both the Individual and Small Group markets:
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.