Massachusetts: Effectuated exchange enrollments up 11% since March
The Massachusetts Health Connector has posted their latest monthly enrollment report (through the end of August), and the news is good. As I note every month:
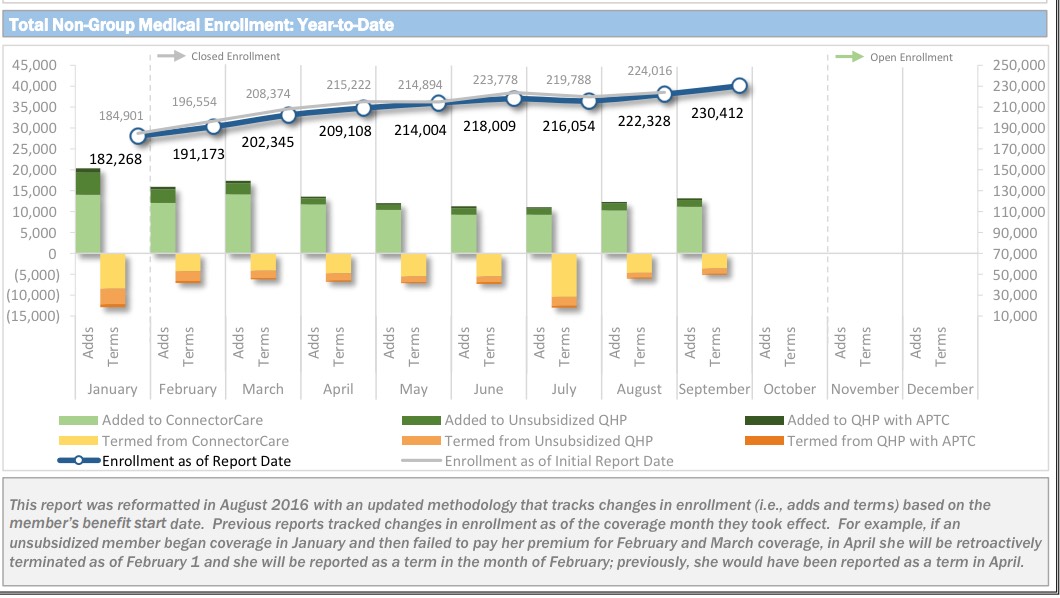
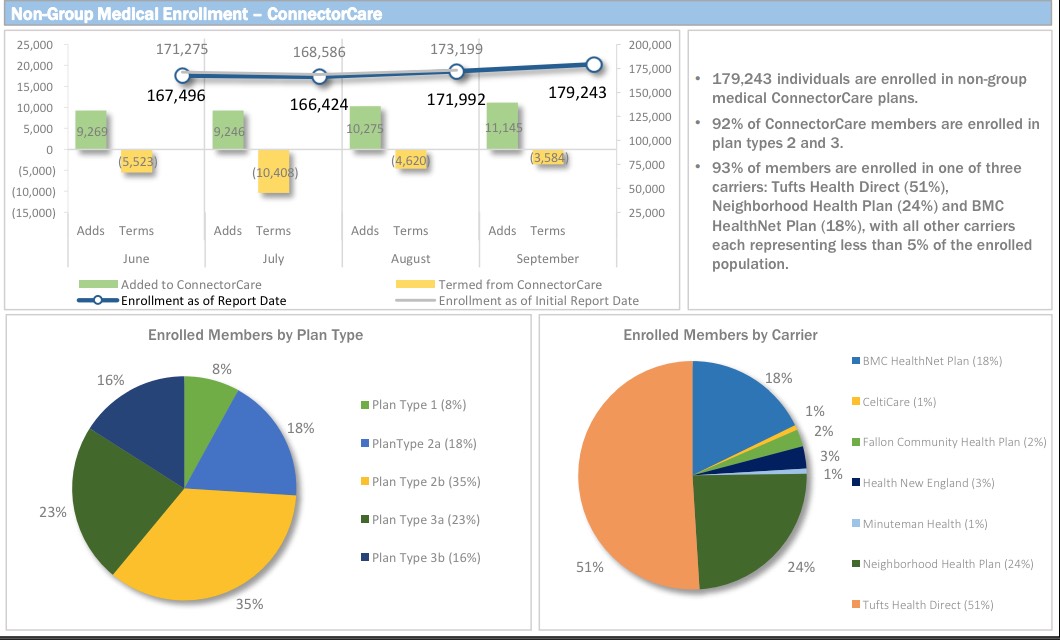
Unlike most states, the Massachusetts Health Connector has not only seen no net attrition since the end of Open Enrollment, but has actually seen a net increase in enrollment...mainly due to their unique "ConnectorCare" policies, which are fully Qualified Health Plans (QHPs) but have additional financial assistance for those who qualify and which are available year-round instead of being limited to the open enrollment period.
The amount of the increase depends on which "official" number you start with; the MA exchange claimed 196,554 people as of 1/31/16...while the ASPE report gives it as 213,883 as of the next day....yet their March report claims 208,000 effectuated enrollees as of February.
Given this discrepancy and the fact that the Q1 2016 effectuated enrollment report has been out for awhile, I'm going to use the 3/31 number (207,121 effectuated enrollees) as the comparison point going forward.
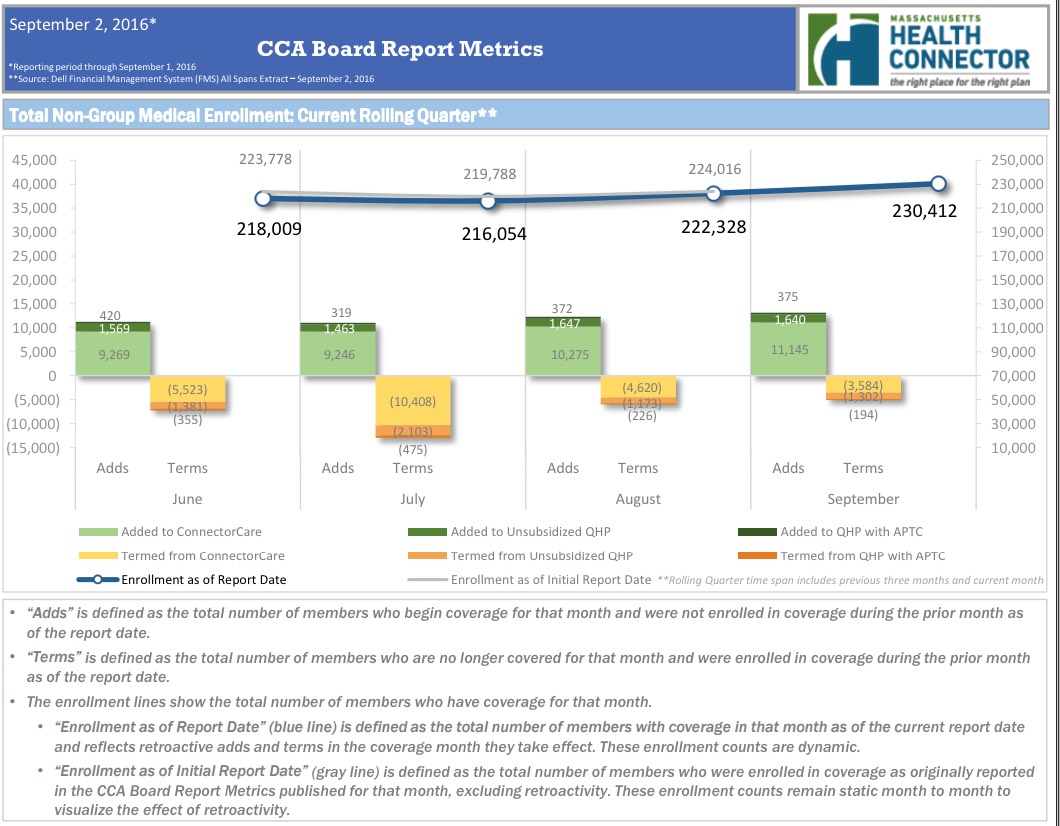
According to the dashboard report, as of September 1st, the MA Health Connector had 230,412 people enrolled in effectuated policies, or 11% more than they had at the end of March.
In addition, there's some other interesting tidbits from the MA board meeting, much of which is very much specific to the Massachusetts population and therefore doesn't necessarily apply to the other 49 states/DC:
- Massachusetts' uninsured rate is down to just 3.6%. Applied to the full population (6.795 million), that's just 245,000 people.
- Based on data on the uninsured and other environmental factors in Massachusetts, the MA exchange identified three groups at higher risk of being uninsured or experiencing gaps in coverage: Latinos, individuals at risk of losing Employer-Sponsored Insurance (ESI) and new Massachusetts residents.
- 1/4 of the remaining uninsured are Latino (7.8% of MA Latinos are uninsured), or around 60,000 Latinos.
- 31% of MA uninsured cite reason as lost job/changed employers; make sure they know about alternatives to COBRA
- 230K new MA residents since 2010
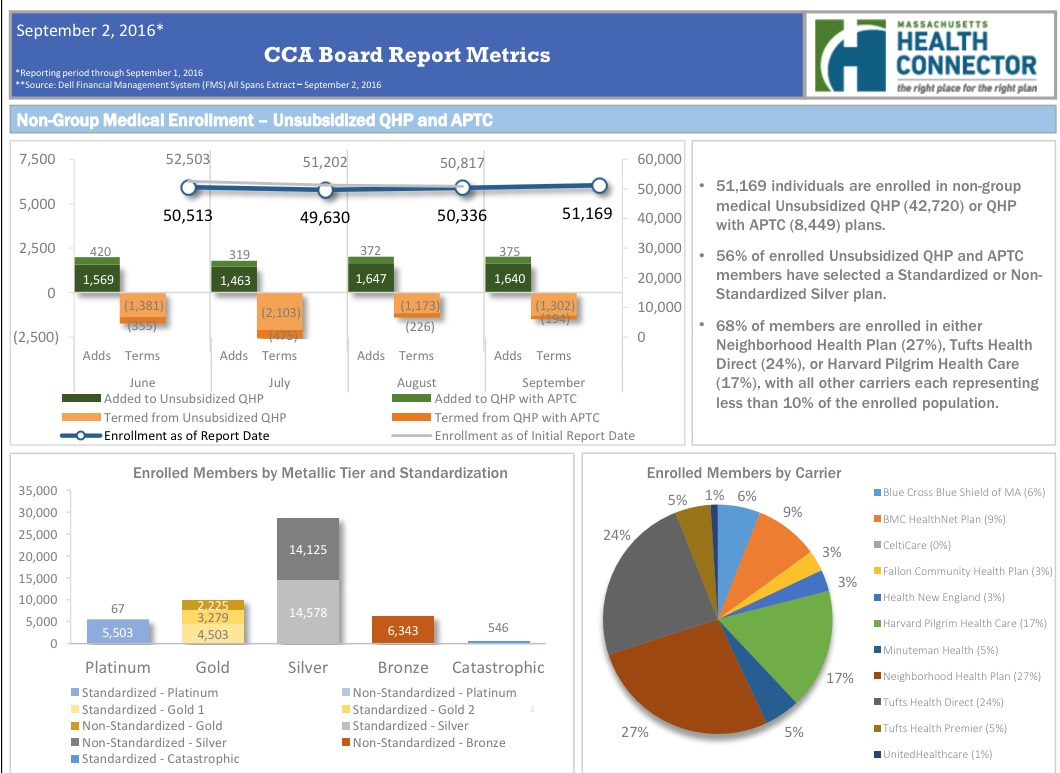
- Some interesting notes about the approved 2017 MA exchange plans; in addition to the normal ACA requirements (and Massachusetts requirements), exchange policies requirements may include:
- Propose one Standardized plan on each metallic tier on broadest commercial network
- Option to propose one alternative network variation for each metallic tier
- Option to propose up to three Non-standardized plans in total
- May request to withdraw Standardized Bronze plan if Health Connector receives a sufficient number of Bronze options
- Propose a Catastrophic plan; may request to withdraw Catastrophic plan if Health Connector receives a sufficient number of Catastrophic options
- Propose a ConnectorCare-compatible Silver plan for the ConnectorCare program that complies with the Health Connector’s network adequacy requirements for this population
- Plans may be offered on an any network type, including a narrower network, or a network that is broader than their standard commercial network
- Propose one Standardized plan on each metallic tier on broadest commercial network
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.



