California: Excellent! Budget deal could eliminate deductibles for ACA enrollees earning <400% FPL!

Last month I posted an explainer about a situation in California which boiled down to a huge pot of extra revenue (~$330 million per year, give or take) being fought over between Governor Gavin Newsom and the Democratically-controlled State Legislature.
The bottom line is that this funding was intended to go towards reducing health insurance premiums for ACA exchange enrollees via Covered California as supplemental subsidies to be added on top of federal ACA tax credits...but the passage of the American Rescue Plan and the subsequent Inflation Reduction Act kind of made that moot, since the federal subsidies were made more generous than what the state subsidies would have been anyway.
As a result, Gov. Newsom decided that the extra revenue should go into the general state fund, while Democrats on the state legislature wanted to redirect it to eliminate deductibles and other types of cost sharing for ACA enrollees instead. This led to an impasse for the past several months:
via Angela Hart of KFF Health News (by way of the Los Angeles Times):
...Democrats, who, then as now, controlled the state Legislature, ultimately backed Newsom in exchange for a promise: The state would levy the fine but use that money to provide financial assistance to offset out-of-pocket costs for Californians purchasing health insurance on the state exchange, Covered California.
Newsom, now in his second term, has since backed off that promise. His administration is holding on to revenue raised from the so-called individual mandate — the requirement that people have health coverage or pay a fine. And his proposed budget for the upcoming fiscal year beginning July 1, which is being debated in the Legislature, funnels the money to the state’s general fund.
That is infuriating fellow Democrats who accuse him of breaking a promise and disregarding the millions of Californians who can’t afford their deductibles and copays.
Fortunately, Newsom and the legislature have now apparently come to a compromise which (while I still side with the legislature's view on principle) seems reasonable to me. Via Amy Lotven of Inside Health Policy:
California will direct a portion of money collected from the state’s coverage mandate to a reserve fund that will be used to lower out-of-pocket costs for Covered California enrollees under a budget deal that is receiving praise from wide-ranging health care stakeholders in the state. Advocates, providers and insurers also applaud a renewed tax on Medicaid managed care organizations that is expected to raise more than $19 billion that will be used to bolster Medi-Cal, including by increasing pay rates for certain providers, although the policy must be approved by the federal government.
...Under the agreement, $82.5 million will be allocated to the health care reserve fund in 2024, and $165 million will go into the reserve in 2025 and beyond.
That's roughly 25% which will go to the healthcare reserve fund this year; it sounds like the funds will be split 50/50 going forward.
The investment could potentially be used to wipe out deductibles to people earning less than 400% of poverty, the advocates say, noting that the deductibles are slated to increase to $5,400 in 2024.
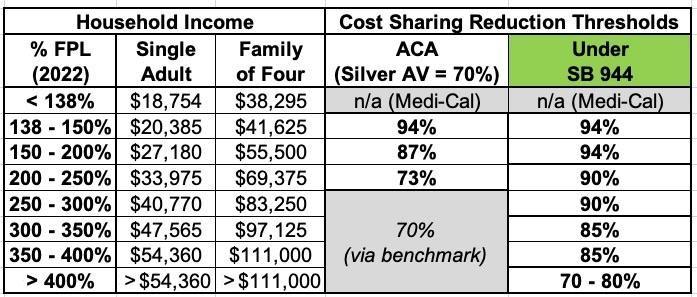
The original proposal from February 2022 hoped to make Cost Sharing Reductions for CoveredCA enrollees far more generous, increasing the Actuarial Value of exchange plans like so:
It sounds to me like the compromise agreement wouldn't necessarily bump the AV levels up quite this high, but it should still dramatically reduce deductibles, co-pays and coinsurance for the vast bulk of ACA exchange enrollees. Nearly 1.5 million of CoveredCA's 1.7 million enrollees earning under 400% FPL, and over 1.1 million earn between 150 - 400% FPL, so this is a Big F*cking Deal.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.