My Unofficial 2019 Open Enrollment Period Projection
I want to stress the unofficial caveat here.
Last year there was an unprecedented amount of uncertainty and chaos surrounding the Affordable Care Act. On the one hand, you had Congressional Republicans desperately attempting to repeal the ACA altogether a good half a dozen times...and coming within a single "thumbs down" of doing so at one point.
At the same time, you had Donald Trump screaming into the wind about doing everything he could to simultaneously cause the ACA exchanges to "blow up" or "implode", depending on the tweet of the day, culminating in him finally pulling the plug on Cost Sharing Reduction reimbursement payments.
Meanwhile, The rest of Trump's lead administrators were doing all they could to undermine, sabotage, or otherwise hinder nearly every aspect of the ACA, from slashing the marketing budget for HealthCare.Gov by 90% and the Navigator/outreach budget by 40% to instructing the IRS not to enforce the individual mandate penalty. Numerous insurance carriers continued the trend of dropping out of the ACA market altogether, with several of them stating point-blank that Trump's CSR cut-off, along with other actions by the administration, were specifically to blame for their decision.
On the other hand, most carriers in most states responded to the CSR cut-off by scrambling to follow California's lead at the last minute and going the #SilverLoading or #SilverSwitcharoo route...in short, they simply jacked up their unsubsidized premiums on Silver plans accordingly to cancel out their CSR losses. This, combined with the fact that most of them had actually broken even or even made a solid profit starting in 2017 (under Obama-era regulations), meant that the damage wasn't as bad as they thought, and the 29% average premium hikes pretty much mitigated or cancelled out the rest of it.
When the dust settled, total 2018 QHP selections came in at 11.75 million people: Around 8.75 million via the 39 states hosted by HealthCare.Gov, plus 3.0 million more in the 12 states operating their own ACA exchanges. This was down roughly 3.8% from the 2017 Open Enrollment Period (OEP) (which in turn was down around 3.7% from 2016).
So what about 2019? Well, there have been additional major developments since last year, and while some will drag enrollment down, others will actually push enrollment up (Dave Anderson has a similar list of factors over at HealthAffairs):
Positive Enrollment Factors:
- Unsubsidized premiums are indeed dropping in a dozen states or so, including Alabama, Alaska, Iowa, Louisiana, Maryland, Minnesota, New Hampshire, North Carolina, Oklahoma, Pennsylvania, Tennessee and Wisconsin. The biggest reasons for this include reinsurance programs being implemented in several states, combined with most of the carriers simply overestimating the fallout from last year's carnage. HOWEVER, it's important to note that this will likely have more of a positive effect on off-exchange ACA enrollment as opposed to on-exchange enrollment, especially in states utilizing the #SilverSwitcharoo gambit...which is most of them.
- Nine states are upgrading their CSR load strategy to go full #SilverSwitcharoo, which should result in bargains galore in four states (Colorado, Delaware, North Dakota and Vermont) and enhanced deals in the other five (Alaska, Arkansas, Kentucky, New Mexico and Tennessee). The downside of this is that unsubsidized Silver enrollees will have to switch to off-exchange Silver plans if they want to avoid the CSR hit, but there should be a net upside for exchange enrollment here.
- As noted above, the fact that they overestimated the damage to the risk pool last fall means that some carriers are doing an about-face and reentering various ACA markets for 2019. This should have some positive impact on enrollment.
Negative Enrollment Factors:
- While premiums dropping in many areas are good news for unsubsidized enrollees, the way ACA subsidies are impacted by benchmark plan premium changes means that many unsubsidized enrollees could be in for a rude awakening as their subsidies drop by more than their premiums. This is also a potential downside of additional carriers entering the market.
- The whole reason that the mandate penalty existed in the first place was to encourage healthier people to stick around in the ACA market, keeping premiums from spiking too much. With the penalty now gone in 48 states (only DC, MA and NJ will have it around for 2019), expect some number of healthier exchange enrollees to bail. How many? I have no idea.
- Related to the above: #ShortAssPlans. The Trump Administration is going hog wild on doling out non-ACA compliant (read: often junk) "short-term, limited duration" plans (which will no longer be either short term nor of limited duration) and "association health plans" (which don't really require you to be part of any serious association). While a dozen or so states will still have significant restrictions on either or both of these, it'll be open season in most states. Expect some number of healthier enrollees to be lured away by these as well. There's also the expansion of "farm bureau" plans which literally aren't even defined as "insurance" in Iowa specifically.
- Finally, there's one enrollment drop factor which is actually a good thing: Medicaid expansion! Virginia has officially expanded the program to around 400,000 residents starting January 1st, of which I estimate around 85,000 likely earn between 100-138% of the Federal Poverty Line and are currently enrolled in heavily-subsidized ACA exchange plans. All of them should be transferred off of their exchange plans over to Medicaid.
- Sidenote: Medicaid expansion also became law earlier this year in Maine and should've been implemented by now, but jackass Governor LePage is being...well, a jackass about it, so it's still sitting idle and will remain that way until the new governor takes office. I estimate around around 12,000 Maine residents will (eventually) make the transition. In addition, I estimate around 80,000 residents of Idaho, Nebraska and Utah combined could be shifted from high-subsidy ACA policies to Medicaid if all three states pass their respective Medicaid expansion ballot initiatives next week. Again, though, implementation of the expansion wouldn't actual happen until several months into 2019, so this won't impact the Open Enrollment Period numbers.
On top of all of this, there are some new major monkey wrenches which have been thrown into the future of the ACA itself. The biggest is the jaw-droppingly stupid #TexasFoldEm federal lawsuit, the complete mangling of the 1332 Waiver rules just announced last week, and of course the 2018 midterm election...which takes place a week after OEP begins. The weird thing is that while the ACA itself is in just as much peril, if not more, than it has ever been to date...the 2019 OEP itself is in some ways less uncertain than it was last year.
To understand how this can be, you have to remember that I'm talking about the immediate future only: The 92-day period from November 1st through January 31st, and especially the 45 days from November 1st - December 15th, which is the enrollment deadline for at least 42 states or so. All hell may break loose after OEP ends, but the insurance carriers should be contractually locked in for the full 2019 calendar year, which means any major fallout from the #TexasFoldEm decision and/or 1332 waiver changes shouldn't really kick in until 2020.
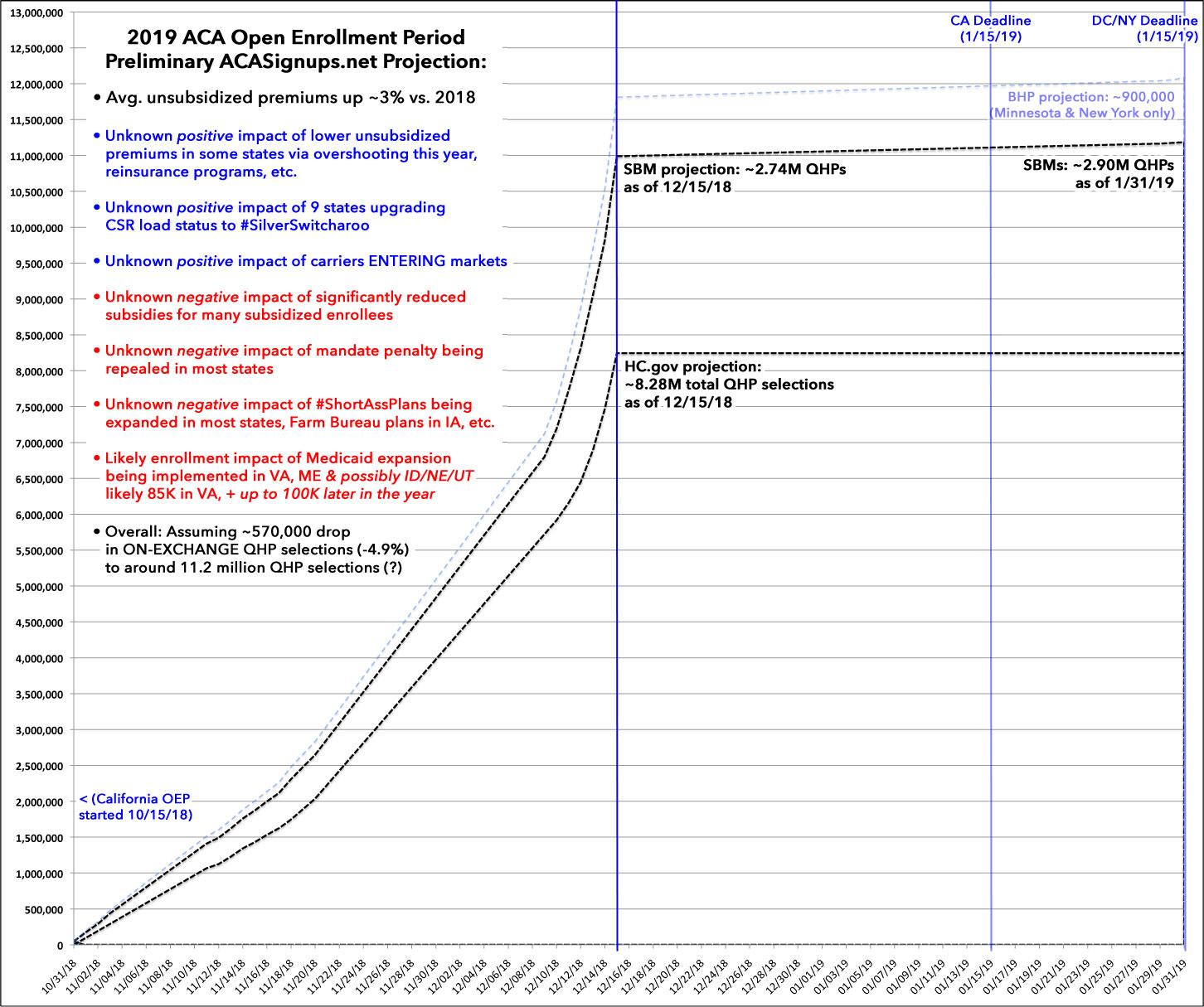
Even so, there are still a lot of unknowns at play tugging the numbers both ways. With all of this in mind, I'm going to go with a spitball estimate of perhaps 11.2 million QHP selections nationally by the time the dust settles on January 31st, 2019. I figure enrollment in the 12 state-based exchanges will only drop slightly (perhaps 100K or so). California, DC, Maryland and Massachusetts all have strict restrictions on short-term plans (or ban them completely); DC and Massachusetts have their own mandate penalty, and so on. In addition, Colorado is upgrading to #SilverSwitcharoo, Maryland and Minnesota have robust reinsurance programs, etc., all of which should mostly mitigate the negative impact.
I expect the 39 HealthCare.Gov states, on the other hand, to see a drop of perhaps half a million people or so. As noted above, Virginia will automatically "lose" around 85,000 exchange enrollees due to implementing their Medicaid expansion program, and although several states on HC.gov do have restrictions on #ShortAssPlans (and New Jersey did implement their own mandate penalty), those compose a much smaller portion of these 39 states.
Again, I have to stress: I could be dead wrong, and wildly so, on any or all of the above. 2019 QHP selections could drop off sharply to 10 million or so...or they could break 12 million again. It's a crapshoot as always.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.