UPDATE x2: Mea culpa: Looks like I botched this one (also, Anthem reverses course in CT)
Via the American Society of Anesthesiologists:
Anthem Blue Cross Blue Shield Won’t Pay for the Complete Duration of Anesthesia for Patients’ Surgical Procedures
CHICAGO – In an unprecedented move, Anthem Blue Cross Blue Shield plans representing Connecticut, New York and Missouri have unilaterally declared it will no longer pay for anesthesia care if the surgery or procedure goes beyond an arbitrary time limit, regardless of how long the surgical procedure takes. The American Society of Anesthesiologists calls on Anthem to reverse this proposal immediately.
Anesthesiologists provide individualized care to every patient, carefully assessing the patient’s health prior to the surgery, looking at existing diseases and medical conditions to determine the resources and medical expertise needed, attending to the patient during the entire procedure, resolving unexpected complications that may arise and/or extend the duration of the surgery, and working to ensure that the patient is comfortable during recovery.
Payment for anesthesia services is based on several factors, including the exact amount of time for anesthesiologists to deliver care preoperatively, during the operation, and when transitioning the patient to the recovery unit afterwards. With this new policy, Anthem will arbitrarily pre-determine the time allowed for anesthesia care during a surgery or procedure. If an anesthesiologist submits a bill where the actual time of care is longer than Anthem's limit, Anthem will deny payment for the anesthesiologist’s care. With this new policy, Anthem will not pay anesthesiologists for delivering safe and effective anesthesia care to patients who may need extra attention because their surgery is difficult, unusual or because a complication arises.
Here's the official policy via Anthem's website:
Anesthesia billed time units — Commercial
Beginning with claims processed on or after February 1, 2025, Anthem will change how it evaluates billed time on professional claims for anesthesia services (that is, CPT® codes 00100 through 01999).
We will utilize the CMS Physician Work Time values to target the number of minutes reported for anesthesia services. Claims submitted with reported time above the established number of minutes will be denied. This update will not change industry standard coding requirements or the American Society of Anesthesiologists’ (ASA) anesthesia formula.
This update will account for anesthesia work time included in the pre-service evaluations, intra-service period, and post-service period. The appropriateness of billing for pre- and post-operation time must be documented and follow the guidelines established by the ASA as to the appropriate time that should be counted and documented.
Exclusions:
- Patients under the age of 22
- Maternity-related care
Resources:
- Frequency Editing — Professional reimbursement policy
- CMS Physician Fee Schedule (PSF) Federal Regulation Notice Final Rule Physician Work Time
- American Society of Anesthesiologists (ASA)
If you disagree with a claim reimbursement decision, please follow the claim dispute process as outlined in the Provider Manual. Documentation to support your request will be required.
If you have questions about this communication or need assistance with any other item, please contact your provider relationship management representative.
Apparently if you're under 22 years old or pregnant you're off the hook for whatever reason.
“This is just the latest in a long line of appalling behavior by commercial health insurers looking to drive their profits up at the expense of patients and physicians providing essential care,” said Donald E. Arnold, M.D., FACHE, FASA. “It’s a cynical money grab by Anthem, designed to take advantage of the commitment anesthesiologists make thousands of times each day to provide their patients with expert, complete and safe anesthesia care. This egregious policy breaks the trust between Anthem and its policyholders who expect their health insurer to pay physicians for the entirety of the care they need.”
ASA urges people concerned about Anthem’s proposal to contact their state insurance commissioner or their state legislator.
In June 2024, Elevance Health, the corporate name for Anthem, reported a 24.12% increase in its year-over-year net income to $2.3 billion and a 24.29% increase in its year-over-year net profit margin.
Now, it is worth noting that the American Society of Anesthesiologists obviously isn't exactly a disinterested party here. Having said that, I find it difficult to believe that there's a systemic issue with anesthesiologists deliberately keeping the meter running beyond what's necessary...especially since keeping a patient under anesthesia carries its own serious medical (and liability) risks as well. Doing that would also necessitate the rest of the surgical staff being in on the scam as well, I would think.
In any event, my guess would be that this new policy should be covered under the No Surprises Act, which is supposed to prohibit either healthcare providers or insurance carriers from billing patients for medical treament/services which the patient couldn't reasonably have been expected to know would be out of network prior to them being performed (such as emergency surgery as well as, say, the surgeon & hospital being in network but the anesthesiologist being out of network).
In those sorts of situations, the No Surprises Act requires the provider and insurance carrier to slug it out between themselves without putting the patient in the middle of the dispute.
UPDATE: Hoo, boy. It looks like I massively botched this one.
On Bluesky, where the ASA's press release was going viral all day today (which I played a part in making happen), a user named Aaron Blackshear took a step back and looked at the outrage more skeptically this evening:
This is not to defend Anthem in any way, but that viral article about anesthesiologists is published by their cartel. There's a reason it's one of the highest paid specialties, and why a very common surprise medical bill is for an out of network anesthesiologist on an in-network surgery
So rail against Anthem for sure, but make sure this cartel knows that when there is a reckoning they are getting a massive haircut
The fact that he used the very example I did re. the No Surprises Act perked my interest, and a little later he followed up:
Read a little bit more about this, and goddammit we're getting played you guys. The original link from the ASA is very dishonest. They are moving to the CMS standard for anesthesia billing. In other words, they are going to pay the same way they do for Medicare and Medicaid.
They are using the CMS Physician Work Time standards for anesthesia. This is almost certainly a result of anesthesiologists padding their bills to get paid more.
Here's some of them whining about it, and complaining about the No Surprises Act, the recent law that prevents them from sending you a huge surprise bill for services you thought were in-network
What this policy change is doing is saying there is a cap on how long you can bill for based on the type of surgery, just like there is when it's someone on Medicare. The days of padding those bills for commercially insured people is over. These docs avg 400k/year.
Also, the original link said they are "arbitrarily" choosing the time, which is a blatant lie. CMS sets these standards, they are not arbitrary. If you are worried about an insurer using these, you should know that it is standard practice in Medicare and has been for a long time.
Somehow I mentally skipped over this critical line even though I reposted the actual policy announcement verbatim:
We will utilize the CMS Physician Work Time values to target the number of minutes reported for anesthesia services.
Going a level deeper into hell: the physician work time RVUs that CMS uses are created by the AMA which does so by surveying the relevant specialty (in this case anesthesiology). Which means they’re mad that they’re being restricted to the time they themselves defined.
The AMA is, of course, the American Medical Association. I have no idea whether the claim above is accurate or not, but it would make sense.
So what's the Physician Fee Schedule?
The PFS is the primary method of payment for enrolled health care providers. Medicare uses the PFS when paying:
- Professional services of physicians and other health care providers in private practice
- Services covered incident to physicians’ services (other than certain drugs covered as incident to services)
- Diagnostic tests (other than clinical laboratory tests)
- Radiology services
And what's the CMS Physician Work Time (PST)?
This final rule addresses:
- changes to the physician fee schedule (PFS);
- other changes to Medicare Part B payment policies to ensure that payment systems are updated to reflect changes in medical practice, relative value of services, and changes in the statute;
- codification of establishment of new policies for, the Medicare Prescription Drug Inflation Rebate Program under the Inflation Reduction Act of 2022;
- updates to the Medicare Diabetes Prevention Program expanded model; payment for dental services inextricably linked to specific covered medical services;
- updates to drugs and biological products paid under Part B including immunosuppressive drugs and clotting factors;
- Medicare Shared Savings Program requirements;
- updates to the Quality Payment Program; Medicare coverage of opioid use disorder services furnished by opioid treatment programs;
- updates to policies for Rural Health Clinics and Federally Qualified Health Centers; electronic prescribing for controlled substances for a covered Part D drug under a prescription drug plan or a Medicare Advantage Prescription Drug (MA-PD) plan under the Substance Use-Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities Act (SUPPORT Act);
- update to the Ambulance Fee This document is scheduled to be published in the Federal Register on 12/09/2024 and available online...
- codification of the Inflation Reduction Act and Consolidated Appropriations Act, 2023 provisions;
- updates to Clinical Laboratory Fee Schedule regulations;
- updates to the diabetes payment structure and PHE flexibilities;
- expansion of colorectal cancer screening and Hepatitis B vaccine coverage and payment;
- establishing payment for drugs covered as additional preventive services;
- Medicare Parts A and B Overpayment Provisions of the Affordable Care Act and Medicare Parts C and D Overpayment Provisions of the Affordable Care Act.
...In accordance with section 1848 of the Social Security Act (the Act), CMS has paid for physicians’ services under the Medicare physician fee schedule (PFS) since January 1, 1992. The PFS relies on national relative values that are established for work, practice expense (PE), and malpractice (MP), which are adjusted for geographic cost variations.
These values are multiplied by a conversion factor (CF) to convert the relative value units (RVUs) into payment rates. The concepts and methodology underlying the PFS were enacted as part of the Omnibus Budget Reconciliation Act of 1989 (OBRA ’89) (Pub. L. 101-239, December 19, 1989), and the Omnibus Budget Reconciliation Act of 1990 (OBRA ’90) (Pub. L. 101-508, November 5, 1990). The final rule published in the November 25, 1991 Federal Register (56 FR 59502) set forth the first fee schedule used for Medicare payment for physicians’ services.
...For anesthesia services, we do not apply adjustments to volume since we use the average allowed charge when simulating RVUs; therefore, the RVUs as calculated already reflect the payments as adjusted by modifiers, and no volume adjustments are necessary. However, a time adjustment of 33 percent is made only for medical direction of two to four cases since that is the only situation where a single practitioner is involved with multiple beneficiaries concurrently, so that counting each service without regard to the overlap with other services would overstate the amount of time spent by the practitioner furnishing these services.
...While flexibility to provide direct supervision through audio/video real-time communications technology was adopted to be responsive to critical needs during the PHE for COVID–19 to ensure beneficiary access to care, reduce exposure risk and to increase the capacity of practitioners and physicians to respond to COVID–19, we expressed concern that direct supervision through virtual presence may not be sufficient to support PFS payment on a permanent basis, beyond the PHE for COVID–19, due to issues of patient safety. For instance, in complex, high-risk, surgical, interventional, or endoscopic procedures, or anesthesia procedures, a patient's clinical status can quickly change; in-person supervision would be necessary for such services to allow for rapid on-site decision-making in the event of an adverse clinical situation. In addition to soliciting comment in the CY 2021 PFS proposed rule on whether there should be any additional ‘‘guardrails’’ or limitations to ensure patient safety/clinical appropriateness, beyond typical clinical standards, as well as restrictions to prevent fraud or inappropriate use, we solicited comment in the CY 2024 PFS proposed rule on whether we should consider extending the definition of direct supervision to permit virtual presence beyond December 31, 2024.
...and so on; the entire document is over 3,000 pages long and covers a lot of medical wonkiness, but it goes into deeply detailed discussion about anesthesia and anesthesiologists (there's over 50 references to them throughout). The larger point is that this is a complex issue which is addressed in depth in official CMS guidelines.
As for Blackshear's claims regarding anesthesiologists being extremely highly-paid, that absolutely bears out; in fact, as ACA Signups regular farmbellpsu notes in the comments below, they charge a median of 5.8x Medicare rates for their services:
Data from 429 273 individual physicians across 54 medical specialties were included. Physician charge-to-Medicare payment ratio ranged between 1.0 and 101.1 across individual physicians, with a median of 2.5 (interquartile range [IQR], 1.8-3.6). The ratio varied across specialties (Table 1), with anesthesiology having the highest median (5.8 [IQR, 4.5-7.9]) and general practice having the lowest (1.6 [IQR, 1.3-2.2]). The ratio also varied across states (Table 2), with state median ranging between 2.0 (IQR, 1.5-3.1 for Michigan) and 3.8 (IQR, 2.9-6.5 for Wisconsin).
Of the 10 730 physicians with high excess charges, 55% were anesthesiologists and 3% were in general practice, internal medicine, or family practice. Of these physicians, 32% practiced in 10 of the 306 hospital referral regions in the United States: East Long Island and Manhattan, New York; Dallas and Houston, Texas; Milwaukee, Wisconsin; Atlanta, Georgia; Camden and Newark, New Jersey; Los Angeles, California; and Charlotte, North Carolina. The total number of physicians practicing in these 10 regions accounted for 16% of all US physicians.
The point of this update isn't to say that Anthem BCBS is actually the Good Guys or that anesthesiologists are suddenly the Bad Guys; it's just that I should have been far more skeptical before instantly leaping to the defense of the ASA or to condemn Anthem on a subject which I clearly wasn't familiar enough with before doing so.
In short, I screwed up bigtime here. My apologies.
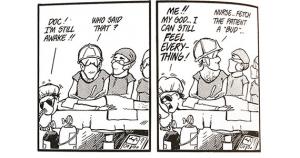
As for the thumbnail above, that's from Bloom County 40 years ago...
UPDATE 12/05/24:
Regardless of whether the backlash is overblown or not, it sounds like it was effective; Anthem now says that they're reversing the time-limit policy in Connecticut, at least, just 24 hours after the story went viral on social media (not sure about the other two states):
An unpopular move to cap anesthesiology coverage by Anthem Blue Cross Blue Shield drew criticism from patients and state officials.
However, Connecticut’s comptroller announced on Thursday that anesthesiology would be covered by Anthem in the state.
Wednesday, Anthem released information about a cap on anesthesia coverage that said if surgery extended past a time limit, it would not be covered.
Comptroller Sean Scanlon said that following conversations with Anthem, the provider for the state employee health plan and many others throughout Connecticut, Anthem will no longer be implementing the policy to limit coverage of anesthesiology.
“After hearing from people across the state about this concerning policy, my office reached out to Anthem, and I’m pleased to share this policy will no longer be going into effect here in Connecticut,” Scanlon said.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.




