"Beware of the Leopard!" ~20% of Medicaid expansion enrollees would likely have no way of reporting their work hours...by design
NOTE: This is an updated version of a blog post I published in 2019 in light of the House GOP's #OneBigUglyBill pending in Congress today.
From The Hitchhiker's Guide to the Galaxy:
But the plans were on display…”
“On display? I eventually had to go down to the cellar to find them.”
“That’s the display department.”
“With a flashlight.”
“Ah, well, the lights had probably gone.”
“So had the stairs.”
“But look, you found the notice, didn’t you?”
“Yes,” said Arthur, “yes I did. It was on display in the bottom of a locked filing cabinet stuck in a disused lavatory with a sign on the door saying ‘Beware of the Leopard.”
From a June 2019 story about Arkansas' "Designed to Fail" Medicaid work requirement disaster:
Under the Arkansas law, targeted enrollees were notified by the state via mail and informational flyers that they were required to work 80 hours a month, participate in another qualifying activity such as job training or community service, or meet criteria for an exemption such as pregnancy, a disability or parenting a child.
If they were out of compliance for three months during a calendar year or failed to report their status to the state through online reports, they could lose coverage.
For the first several months of its new mandate, Arkansas required enrollees to use an online portal for that reporting, a problem since 20% lacked internet access and another 20% lacked fast broadband. The state online portal also was unavailable after 9 p.m. each day.
The study found one-third of individuals subject to the policy had not heard anything about it, and 44% were unsure whether the requirements applied to them.
Six years later, from a June 2025 OpEd in the NY Times about the Arkansas fiasco, written by the attorneys who sued to stop the requirements:
Our clients ran the gamut of low-wage work: fast food workers, restaurant dishwashers and servers, construction workers, janitors, landscapers, motel cleaners, gas station clerks and nursing assistants. Many had disabilities, and their ability to continue working depended on getting treatment to manage chronic pain, asthma, injuries, cancer and mental health conditions. Some lost coverage simply because they couldn’t navigate the policy’s complicated requirements and labyrinthine reporting process. Others lost insurance because of the instability of low-wage work: Bosses cut their hours or laid them off without warning, limited public transit narrowed their options or they lived in struggling rural areas where jobs were hard to come by. When the state cut them off, their health worsened and many lost jobs, as well as the ability to work new ones.
Nobody on Medicaid was free from the tumult. Despite outreach from the state, there was widespread panic, as people didn’t know if they had the type of Medicaid that the new requirements applied to. People received confusing 10-page letters from the state Medicaid office, which often contradicted other coverage letters people received around the same time. The website to report compliance shut down every night at 9 p.m., and when it was running, it was so complex that we put together video tutorials to help people navigate it successfully. (Many still couldn’t.) People spent hours on the phone or at agency offices trying to figure out their status or fix errors, often needing a lawyer’s help. In some cases, they had to pester their employers for extra proof of wages or statements that met the state’s requirements. All told, 18,164 people were terminated because of noncompliance with the work requirements, and thousands more people lost coverage because of related paperwork burdens.
The OpEd goes on to discuss the false hope of advanced technology solving these problems, but there's another tech-related point I wanted to explore further: Computer ownership & internet access. The first story is from 2019 and technological adoption moves quickly, so I decided to find more recent data.
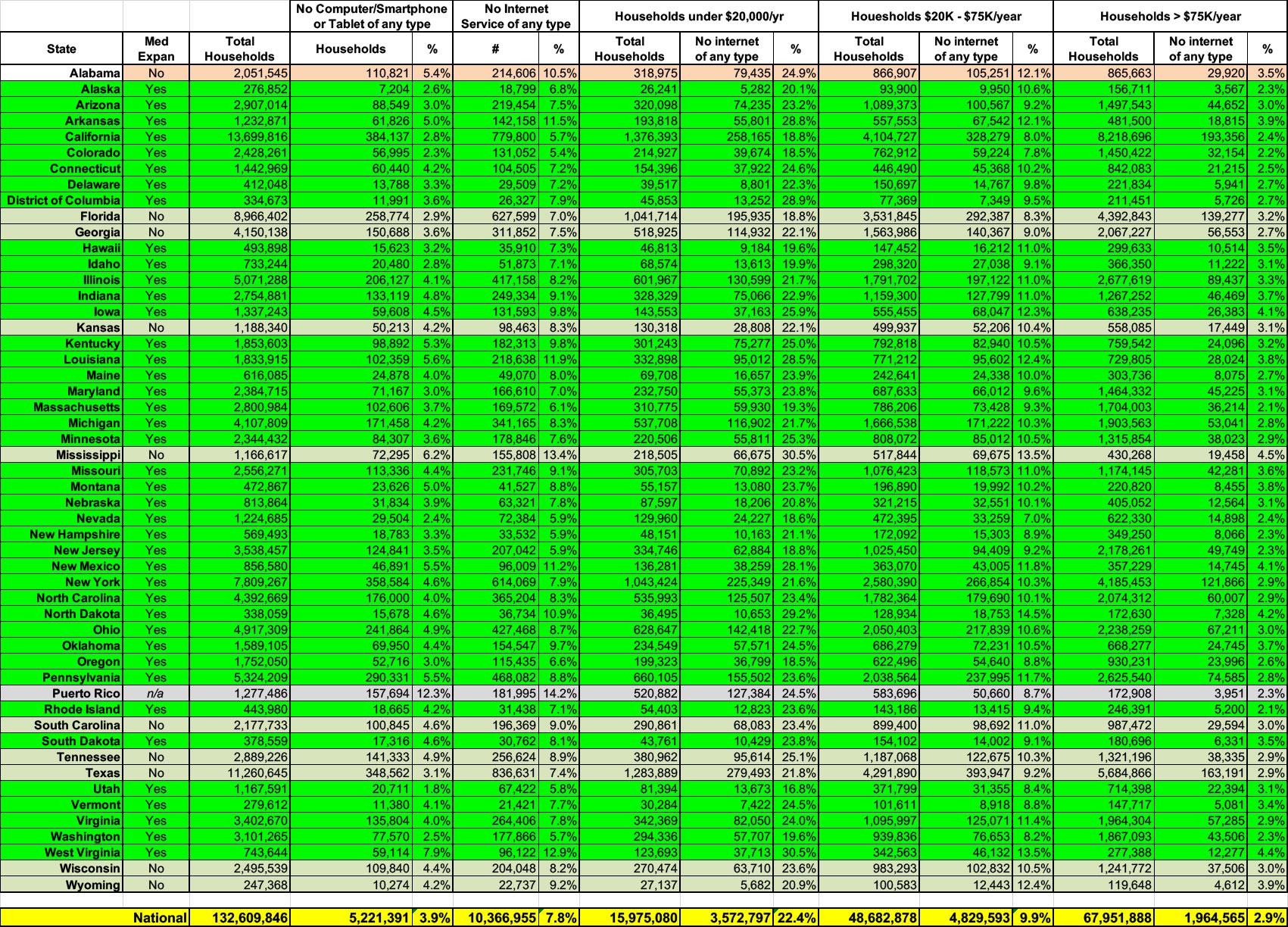
The most recent reliable, relevant source I could find is the American Community Survey by the U.S. Census Bureau from 2023. That's still 2 years out of date but it'll have to do.
Anyway, according to the ACS, over 5.2 million U.S. households--3.9% of the total--still didn't have any computer of any sort as of 2023--that means no laptops, desktops, smartphones or tablets of any kind.
In addition, over 10.3 million households--7.8% of the total still had no internet service of any type--broadband, DSL, satellite, fiber optic, cellular data or even dial-up.
The table below breaks this out by state.
If you limit this to the 40 states (+DC) which have expanded Medicaid under the ACA, the total percentages are roughly the same, but they vary widely by state.
The expansion states with the highest percent of households without any type of computer are West Virginia (7.9%), GOP Speaker of the House Mike Johnson's home state of Louisiana (5.6%) and Arkansas (5.0%).
The expansion states with the highest percent of households without any type of internet service are, once again, West Virginia (12.9%), Louisiana (11.9%) and Arkansas (11.5%).
Remember, however, that these stats include all U.S. households of any income level; Medicaid expansion enrollees have to earn less than 138% of the Federal Poverty Level (FPL), which is $21,597/yr for a single adult, $29,187 for two people, $36,777 for three and $44,367/year for four.
While the ACS doesn't break out the computer ownership data by income level, it does do so for internet access: Households below $20,000/year, households between $20,000 - $75,000/year and households earning more than $75,000/year.
Pretty much every legally-residing adult in these states earning less than $20,000 should be enrolled in Medicaid (although not all of them will be enrolled via ACA expansion; pregnant women, seniors, the disabled etc. are presumably enrolled in traditional Medicaid, while children are likely enrolled in the CHIP program).
The $25K - $75K category is more difficult to parse--a single adult in that income range wouldn't be part of the expansion population, but a couple might (the cut-off for 2 people is $29,187/year), and a couple with children also might (it's $36,777 for 3 people and $44,367 for four). I'd estimate perhaps 1/3 of this population falls below the 138% FPL threshold, though if someone provides a better estimate I'm all ears.
The $75K+ household population obviously would have very few (if any) Medicaid expansion enrollees...even a couple with 6 kids (8 people total) wouldn't qualify at $75K/year; this would be a nominal number.
According to the 2023 ACS, a whopping 22.3% of households earning less than $20K/year didn't have any type of internet service (or nearly 2.45 million), while 10.1% of households in the $25K - $75K range didn't (3.39 million). Adding 1/3 of the $25K-$75K group, that means at least 3.6 million households with at least one Medicaid expansion enrollee would have no obvious way of reporting their "compliance" hours.
Since at least some of those households have more than one person enrolled in Medicaid via ACA expansion, it likely means more like 4 million actual enrollees.
That's 20% of the Medicaid expansion population.
Now, it's true that this data is 2 years out of date; presumably the percentages have shrunk a bit more since then. And of course I suppose you could argue that enrollees could use a public computer at their local library (although the Trump Administration is also attempting to slash funding for those as well).
On the other hand, I'm not even touching issues like having a computer but it being broken/infected; having internet service but it being spotty/unreliable; not having transportation to the library, and so forth. So I'd call the 3.6 million household estimate a pretty good ballpark.
I'm also not sure it's a great idea to be using a public computer to submit personal financial/employment data.
Also, even among the 96% of total households which do have at least one "computer," the ACS reports that 10% have a smartphone only. iPhone/Android phones are extremely powerful these days, of course, but unless the state makes sure that their reporting website has a mobile-friendly interface (or goes the extra mile to develop a dedicated, user-friendly app), it can be a royal pain in the ass to submit complex personal data on a smartphone.
Finally, the ACC survey said there were still 166,000 U.S. households which had dial-up only internet service as of 2023...66,000 of which likely earn less than 138% FPL.
Using my "1/3 of the 2nd population" estimate, there are five states where over 20% of likely Medicaid expansion households have no internet service of any type (West Virginia, Louisiana, North Dakota, Arkansas and New Mexico). The District of Columbia would also rank up there, except they have a special traditional Medicaid enrollment waiver which covers residents earning up to 210% FPL anyway, so I'm not sure that this math would apply there.
Once again: The entire point of imposing "work requirements" on the Medicaid population in the One Big Ugly Bill is specifically to reduce federal spending on Medicaid. The only way to do that is to kick people off of the program, and since the goal is to "save" several hundred billion dollars, that means having to kick millions of people off. That, in turn, means deliberately making the "reporting requirements" as onerous and difficult to comply with as possible.