CMS: ~3.7 Million of those kicked off of Medicaid enrolled in #ACA exchange plans or BHPs thru December
Normally, states will review (or "redetermine") whether people enrolled in Medicaid or the CHIP program are still eligible to be covered by it on a monthly (or in some cases, quarterly, I believe) basis.
However, the federal Families First Coronavirus Response Act (FFCRA), passed by Congress at the start of the COVID-19 pandemic in March 2020, included a provision requiring state Medicaid programs to keep people enrolled through the end of the Public Health Emergency (PHE). In return, states received higher federal funding to the tune of billions of dollars.
As a result, there are tens of millions of Medicaid/CHIP enrollees who didn't have their eligibility status redetermined for as long as three years.
With the end of this continuous coverage as of March 31st, 2023, healthcare advocates have been warning that millions of people would lose coverage, including many who are still actually eligible...and sure enough, as of this week, at least 19.1 million Medicaid enrollees have lost coverage so far, of whom a stunning 70% (13.4 million) were kicked off the program for purely procedural reasons--that is, failure to return a form or, in some cases, state administrations either mistakenly or deliberately sweeping entire families off the programs if a single member is no longer eligible.
The good news is that this doesn't mean that all 19.1 million of these folks are uninsured now. Some of them have moved to employer coverage, Medicare or even rejoined Medicaid/CHIP after re-applying & being found to be eligible after all (in some cases they're no longer eligible via one criteria but are now eligible via a different one, like people in South Dakota and North Carolina which each expanded Medicaid mid-year).
Others are applying for and enrolling in ACA exchange coverage, often heavily subsidized.
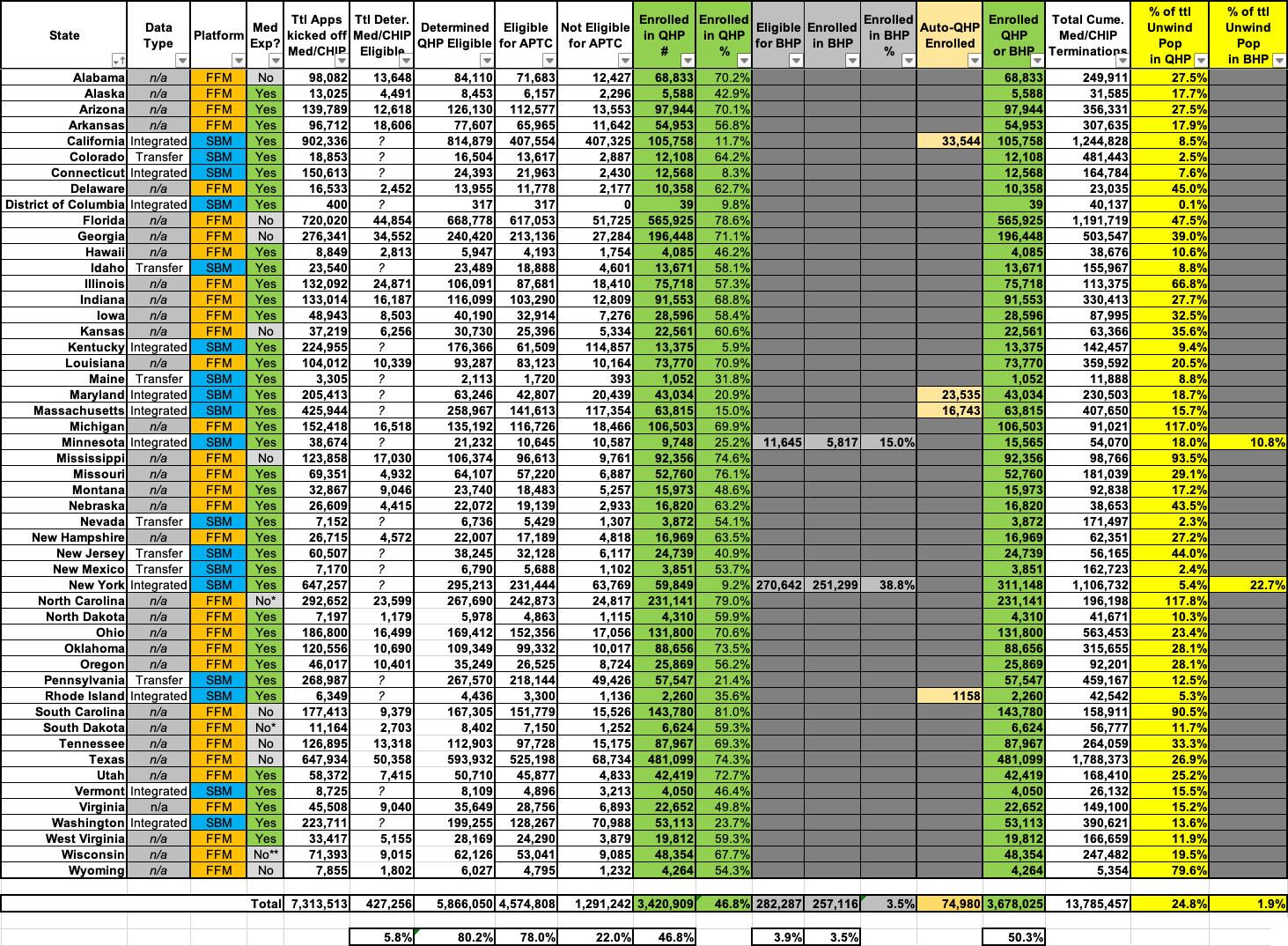
The Centers for Medicare & Medicaid Services (CMS) have been tracking how many of the Unwinding population are applying for, qualifying for and actually enrolling in ACA exchange coverage, and is posting updated reports monthly; the newest one includes data through the end of December:
- Across the 33 states hosted via HealthCare.Gov in 2023 (Virginia moved to their own exchange this year), ~4.1 million of the people who were kicked off of Medicaid/CHIP applied for ACA exchange coverage
- Of those, ~427K (10.4%) were determined by HC.gov to still be eligible for Medicaid/CHIP and presumably have been re-enrolled
- Another ~3.64M (89%) were determined by HC.gov to be eligible for an ACA exchange Qualified Health Plan (QHP), with or without subsidies
- 3.22M were eligible for subsidies; 413K weren't
- Of those, 2,936,460 (71.8% of the total who applied) actually enrolled in a QHP
The state-based exchange report is laid out little differently:
- Across the 18 states which operated their own state-based ACA exchange in 2023, ~3.22 million of the people who were kicked off of Medicaid/CHIP applied for ACA exchange coverage.
- Of those, ~282K (8.8%) were determined eligible for a Basic Health Plan program in Minnesota or New York; 257K (8.0%) actually enrolled in a BHP plan
- Another ~2.23M (69.1%) were determined eligible for an ACA exchange Qualified Health Plan (QHP), with or without subsidies
- 1.35M were eligible for subsidies; 878K weren't
- Of those, 484,449 (15.0% of the total who applied) actually enrolled in a QHP
Across all 50 states +DC, that's 3,420,909 who actually enrolled in a QHP through the end of October, plus the 257,116 BHP enrollees for 3,678,025 total.
Overall, that's 50.3% of the 7,313,513 people who applied for ACA marketplace coverage through August. Another 427K (at least) were determined to still be Medicaid/CHIP eligible, leaving ~3.21 million who had to find some other type of coverage.
It's also important to note that this obviously does not mean that only ~7.31 million Americans had lost Medicaid/CHIP coverage through the end of October. Remember, this only includes those who actually applied for coverage to begin with.
The Medicaid and CHIP National Summary of Renewal Outcomes – March through December 2023 report specifies that a total of 13,785,457 Medicaid/CHIP enrollees were terminated from their coverage from March - December.
This means that through the end of December (which included nearly all of the 2024 ACA Open Enrollment Period), 24.8% of the total Unwinding population enrolled in ACA exchange coverage and another 1.9% enrolled in BHP coverage, or 26.7% total.
If you further extrapolate that out to the 19.1 million people who have been disenrolled as of March 26th, it means the number who have moved to exchange QHPs or BHP coverage is up to perhaps 5.1 million as of today, although the end of the Open Enrollment Period in January likely means the actual number is likely lower than that.
There's also still a strange disconnect between the ratios of HC.gov and SBM states here: 71.8% of HC.gov applicants enrolled in QHPs, while only 23.0% of SBM applicants enrolled in either QHPs or BHPs. Huh.
I've reformatted most of the relevant data into a simplified, easier-to-follow spreadsheet with all 50 states +DC. Some additional takeaways:
- Nearly 75,000 people in 4 states (CA, MD, MA & RI) which have the capability have been automatically transferred from Medicaid/CHIP over to ACA exchange plans.
- Nationally, just over 50% of the Unwinding population who applied for coverage via their ACA exchange have actually enrolled in a QHP or BHP.
- The percentage ranges widely, from as little as 5.9% in Kentucky to as much as 81% in South Carolina.
- Nationally, out of everyone in the Unwinding population thru September, 24.8% enrolled in exchange QHPs and another 1.9% enrolled in BHPs.
- This percentage ranges from as low as 0.1% in DC (where Medicaid eligibility extends all the way up to 210% FPL anyway) to as high as...over 100% in Michigan & North Carolina (117% & 118% respectively), which would be pretty impressive if it wasn't mathematically impossible...
(I'll have to look into this data...)
- Only 78% of those determined eligible for QHPs were also deemed eligible for APTC subsidies. This is noteworthy because it's significantly lower than the 92.1% of all ACA exchange enrollees who receive subsidies. It suggests that either a disproportionately high portion of the Unwinding population is higher income (which makes sense) or that those most likely to actually apply in the first place are higher income, which is rather counterintuitive. Unfortunately the report doesn't break out the APTC/no APTC numbers of those who actually enrolled in QHPs, however.
- 34.8% of the total Unwinding population has enrolled in QHPs in states on the federal exchange vs. 13.9% in QHPs/BHPs in states operating their own exchanges.
- 40.4% of the total Unwinding population had enrolled in QHPs in states which hadn't expanded Medicaid vs. 19.3% in QHPs/BHPs in states which have expanded Medicaid.
- An additional 1.15 million members of the Unwinding population moved from Medicaid/CHIP to QHPs or BHPs in December specifically.