CMS Report: 1.2 Million of those kicked off of Medicaid enrolled in #ACA exchange plans or BHPs thru September
Normally, states will review (or "redetermine") whether people enrolled in Medicaid or the CHIP program are still eligible to be covered by it on a monthly (or in some cases, quarterly, I believe) basis.
However, the federal Families First Coronavirus Response Act (FFCRA), passed by Congress at the start of the COVID-19 pandemic in March 2020, included a provision requiring state Medicaid programs to keep people enrolled through the end of the Public Health Emergency (PHE). In return, states received higher federal funding to the tune of billions of dollars.
As a result, there are tens of millions of Medicaid/CHIP enrollees who didn't have their eligibility status redetermined for as long as three years.
With the end of this continuous coverage as of March 31st, 2023, healthcare advocates have been warning that millions of people would lose coverage, including many who are still actually eligible...and sure enough, as of this week, at least 13.38 million Medicaid enrollees have lost coverage so far, of whom a stunning 71% (9.5 million) were kicked off the program for purely procedural reasons--that is, failure to return a form or, in some cases, state administrations either mistakenly or deliberately sweeping entire families off the programs if a single member is no longer eligible.
The good news is that this doesn't mean that all 13.4 million of these folks are uninsured now. Some of them have moved to employer coverage, Medicare or even rejoined Medicaid/CHIP after re-applying & being found to be eligible after all (in some cases they're no longer eligible via one criteria but are now eligible via a different one, like people in South Dakota and (starting tomorrow) North Carolina which have expanded Medicaid mid-year).
Others are applying for and enrolling in ACA exchange coverage, often heavily subsidized.
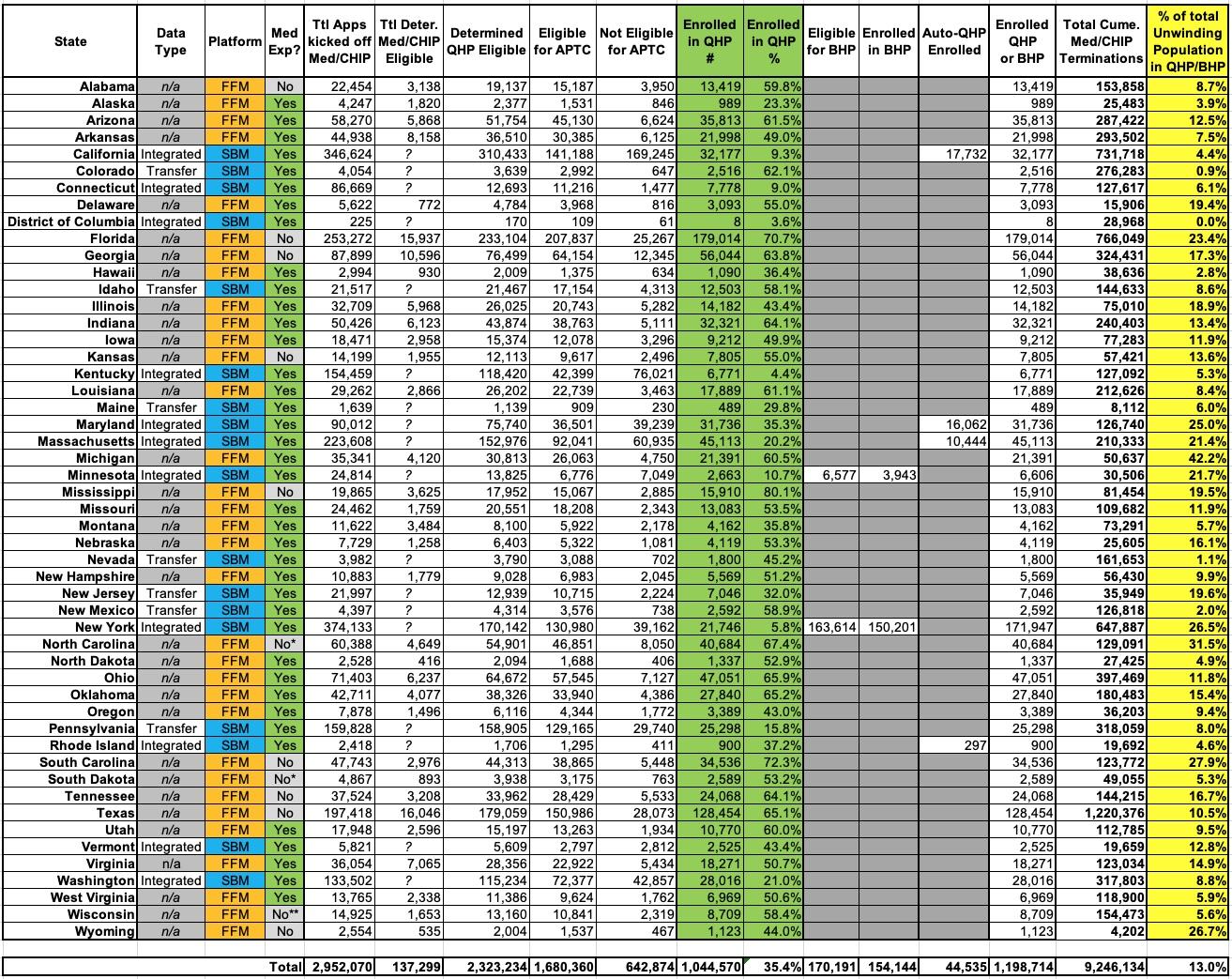
The Centers for Medicare & Medicaid Services (CMS) have been tracking how many of the Unwinding population are applying for, qualifying for and actually enrolling in ACA exchange coverage, and is posting updated reports monthly; the newest one includes data through the end of August:
- Across the 33 states hosted via HealthCare.Gov, ~1.29 million people who were kicked off of Medicaid/CHIP applied for ACA exchange coverage
- Of those, ~137K (11%) were determined by HC.gov to still be eligible for Medicaid/CHIP and presumably have been re-enrolled
- Another ~1.14M (88%) were determined by HC.gov to be eligible for an ACA exchange Qualified Health Plan (QHP), with or without subsidies
- 975K were eligible for subsidies; 165K weren't
- Of those, 812,893 (63% of the total who applied) actually enrolled in a QHP
The state-based exchange report is laid out little differently:
- Across the 18 states which operated their own state-based ACA exchange, ~1.66 million people who were kicked off of Medicaid/CHIP applied for ACA exchange coverage.
- Of those, ~170K (10%) were determined eligible for a Basic Health Plan program in Minnesota or New York; 154K (9.3%) actually enrolled in a BHP plan
- Another ~1.18M (71%) were determined eligible for an ACA exchange Qualified Health Plan (QHP), with or without subsidies
- 705K were eligible for subsidies; 478K weren't
- Of those, 231,677 (14% of the total who applied) actually enrolled in a QHP
Across all 50 states +DC, that's 1,044,570 who actually enrolled in a QHP through the end of September, plus the BHP enrollees for a total of 1,198,714 total.
Overall, that's 40.6% of the 2,952,070 people who applied for ACA marketplace coverage through August. Another 137K (at least) were determined to still be Medicaid/CHIP eligible, leaving ~1.62 million who had to find some other type of coverage.
It's also important to note that this obviously does not mean that only ~2.95 million Americans had lost Medicaid/CHIP coverage through the end of August. Remember, this only includes those who actually applied for coverage to begin with.
The Medicaid and CHIP National Summary of Renewal Outcomes – March through September 2023 report specifies that a total of 9,246,134 Medicaid/CHIP enrollees were terminated from their coverage from March - September 2023.
This means that through the end of September, 11.3% of the Unwinding population enrolled in ACA exchange coverage and another 1.7% enrolled in BHP coverage, or 13.0% total.
If you further extrapolate that out to the 13.38 million people who have been disenrolled as of December 20th, it means the number who have moved to exchange QHPs is up to perhaps 1.51 million as of today, plus perhaps another 223K BHP enrollees...call it perhaps 1.73 million total.
It may seem surprising at first that there are more people in state-based exchange states who lost coverage given that only 40% of the total U.S. population lives in those states, but keep in mind that all of the state-based exchange states have expanded Medicaid under the ACA, while 10 of the HC.gov states haven't done so (including huge states like Texas and Florida), meaning they generally had a higher portion of their residents in Medicaid/CHIP in the first place.
There's also still a strange disconnect between the ratios of HC.gov and SBM states here: 63% of HC.gov applicants enrolled in QHPs, while only 23% of SBM applicants enrolled in either QHPs or BHPs. Huh.
I've reformatted most of the relevant data into a simplified, easier-to-follow spreadsheet with all 50 states +DC. Some key takeaways:
- Over 44,000 people in 4 states (CA, MD, MA & RI) which have the capability have been automatically transferred from Medicaid/CHIP over to ACA exchange plans.
- Nationally, 35.4% of the Unwinding population who applied for coverage via their ACA exchange have actually enrolled in a QHP, plus another 5.2% in MN/NY who enrolled in BHP plans
- The percentage ranges widely, from as little as 3.6% in DC to as much as 80.1% in Mississippi.
- Nationally, out of everyone in the Unwinding population thru September, 11.3% enrolled in exchange QHPs and another 1.7% enrolled in BHPs.
- This percentage ranges from as low as 0% in DC (where Medicaid eligibility extends all the way up to 210% FPL anyway) to as high as 42.2% here in Michigan, which is pretty impressive!
- Only 72.3% of those determined eligible for QHPs were also deemed eligible for APTC subsidies. This is noteworthy because it's significantly lower than the 90.5% of all ACA exchange enrollees who are receiving subsidies. It suggests that either a disproportionately high portion of the Unwinding population is higher income (which makes sense) or that those most likely to actually apply in the first place are higher income, which is rather counterintuitive. Unfortunately the report doesn't break out the APTC/no APTC numbers of those who actually enrolled in QHPs, however.
- 14.0% of the total Unwinding population has enrolled in QHPs in states on the federal exchange vs. 11.2% in QHPs/BHPs in states operating their own exchanges.
- 16.0% of the total Unwinding population had enrolled in QHPs in states which hadn't expanded Medicaid as of this summer (ie, including NC & SD) vs. 11.4% in QHPs/BHPs in states which have expanded Medicaid.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.