Oh, good: CMS reinstating Medicaid/CHIP coverage for half a million kids & adults kicked off by mistake
Three weeks ago, the Centers for Medicare & Medicaid Services (CMS) announced that they were cracking down on one of the main reasons why so many people are being kicked off of Medicaid and the Children's Health Insurance Program (CHIP) even though they were still eligible:
CMS believes that eligibility systems in a number of states are programmed incorrectly and are conducting automatic renewals at the family-level and not the individual-level, even though individuals in a family may have different eligibility requirements to qualify for Medicaid and CHIP. For example, children often have higher eligibility thresholds than their parents, making them more likely to be eligible for Medicaid or CHIP coverage even if their parents no longer qualify. This conflicts with existing federal Medicaid requirements and may have a disproportionate impact on children.
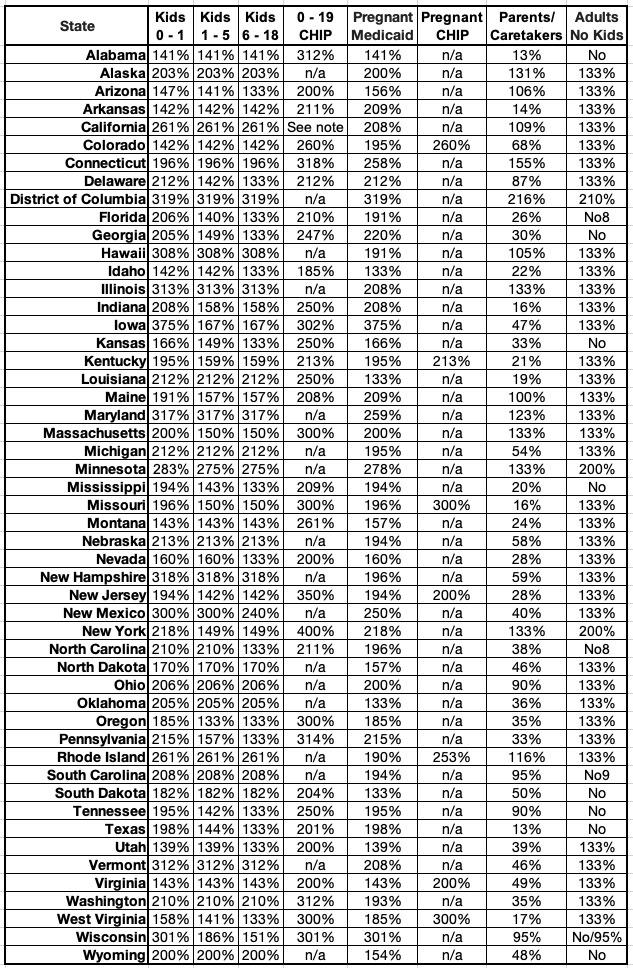
Again, here's the income eligibility thresholds for different groups of people by state. As you can see, there's eight different categories...and the household income cut-off for children runs as high as 350% of the federal poverty level (FPL) in New Jersey, while in some states their parents are only eligible at incomes as low as 13% FPL in Alabama and Texas (this may actually be 18% if it includes the same 5% income disregard that ACA expansion does):
Today CMS has issued their findings, and while it's pretty forehead-slappingly stupid that this has been happening in the first place, the good news is that it sounds like the error is at least being corrected:
Coverage for Half a Million Children and Families Will Be Reinstated Thanks to HHS’ Swift Action
- CMS Requires States to Pause Disenrollments and Reinstate Coverage for Impacted Individuals
Today, the U.S. Department of Health and Human Services (HHS) is announcing that it has helped half a million children and families regain their Medicaid and Children’s Health Insurance (CHIP) coverage. On August 30, the Centers for Medicare & Medicaid Services (CMS) issued a call to action to states about a potential state systems issue where systems were inappropriately disenrolling children and other enrollees, even when the state had information indicating the person remained eligible.
Thanks to CMS’ swift action, nearly 500,000 children and other individuals who were improperly disenrolled from Medicaid or CHIP will regain their coverage, and many more are expected to be protected from improper disenrollments going forward.
CMS sent a letter on August 30 to all states, the District of Columbia, Puerto Rico, and the U.S. Virgin Islands requiring them to determine and report whether they have a systems issue that inappropriately disenrolls children and families, even when the state had information indicating that they remained eligible for Medicaid and CHIP coverage. Today’s summary indicates that to-date 30 states report having this systems issue. As a result, to avoid CMS taking further action, all 30 states were required to pause procedural disenrollments for impacted people unless they could ensure all eligible people are not improperly disenrolled due to this issue.
“Thanks to swift action by HHS, nearly half a million individuals, including children, will have their coverage reinstated, and many more will be protected going forward. HHS is committed to making sure people have access to affordable, quality health insurance – whether that’s through Medicare, Medicaid, the Marketplace, or their employer,” said HHS Secretary Xavier Becerra. “We will continue to work with states for as long as needed to help prevent anyone eligible for Medicaid or CHIP coverage from being disenrolled.”
“Medicaid and CHIP are essential for millions of people and families across the country,” said CMS Administrator Chiquita Brooks-LaSure. “Addressing this issue with auto-renewals is a critical step to help eligible people keep their Medicaid and CHIP coverage during the renewals process, especially children. CMS will keep doing everything in our power to help people have the health coverage they need and deserve.”
CMS’ letter on August 30 alerted states to a potential eligibility systems issue related to automatic renewals for Medicaid and CHIP coverage. Auto-renewals (also known as “ex parte” renewals) are one of the strongest tools that states have to keep eligible people enrolled in Medicaid or CHIP coverage during the renewals process. Federal rules require states to use information already available to them through existing reliable data sources (e.g., state wage data) to determine whether people are still eligible for Medicaid or CHIP. Auto-renewals make it easier for people to renew their Medicaid and CHIP coverage, helping to make sure eligible individuals are not disenrolled due to red tape. CMS continues to provide technical assistance to states as they address these system issues.
Throughout the renewals process, CMS has offered states many strategies to assist them in making it easier for people to renew their coverage. Nearly all states have adopted at least some of these strategies, and CMS continues to urge states to adopt these strategies. Additionally, to help make transitions from Medicaid to other health coverage options more accessible in every state, CMS has launched national marketing campaigns and made available Special Enrollment Periods through HealthCare.gov, State-based Marketplaces, and Medicare. CMS’ top priority remains making sure everyone has access to affordable, quality health coverage.
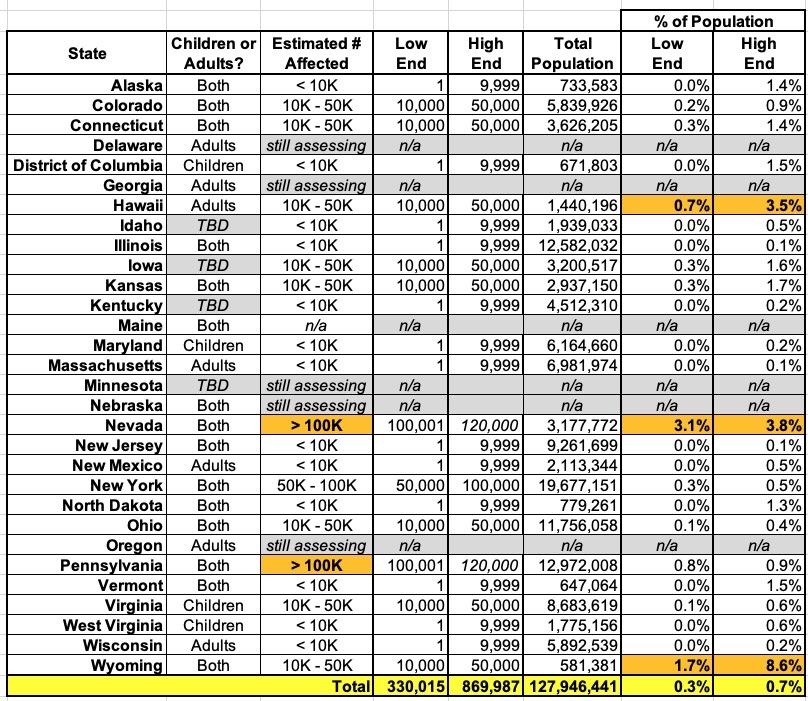
Here's a simplified version of the state-by-state overview, listing which types of enrollees were impacted and a rough estimate of how many have been kicked off improperly in each state. As you can see, in 12 states there were fewer than 10,000 people who lost coverage; in 8 states it ranges from 10,000 - 50,000. It's somewhere between 50K - 100K in New York, and both Nevada and Pennsylvania appear to have wrongly terminated over 100,000 residents from Medicaid or CHIP coverage.
Keep in mind that Nevada only has about 3.2 million people total, so that's between 3.1% - 3.8% of the entire state population. Wyoming is even more of a jaw-dropper, however: They only have ~580,000 residents, yet has removed between 10K - 50K of them from their Medicaid/CHIP roles...or somewhere betwen 1.7% - 8.6% of their entire population. Yikes.
Again, the good news is that hopefully these folks will have their coverage reinstated ASAP.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.