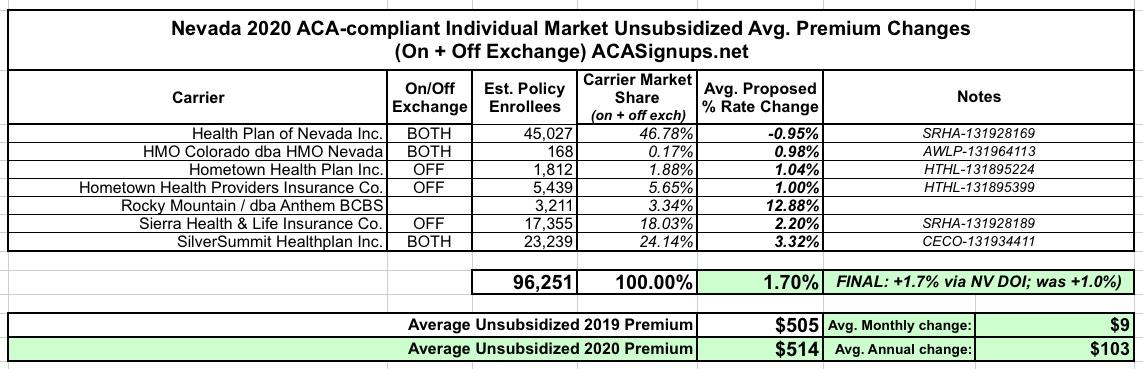
Nevada: *Final* avg. 2020 #ACA rate changes: 1.7% increase
In early August, the Nevada Dept. of Insurance posted the state's preliminary 2020 individual market rate changes. The data was a bit incomplete and confusing, but the bottom line is that average unsubsidized 2020 premiums were only expected to increase about 1.0%.
Today they posted the final/approved rate changes, and unlike most states, the overall weighted average will be slightly higher than the original numbers...although only by a hair:
Nevada Division of Insurance reveals approved 2020 Health Insurance Rates
Carson City, NV – The Division of Insurance (‘Division”) has posted the approved 2020 health insurance rates for all plans in the Individual Health Insurance Market at healthrates.doi.nv.gov and encourages consumers to review this information before the Open Enrollment Period begins.
For 2020, consumers have the option of buying health insurance from a total of seven insurance companies offering as many as 60 plans on and off the Exchange in the individual health insurance market in Nevada. The approved average rate increase in the individual market, both on and off the Exchange is 1.7%
There are three insurance companies offering plans on the Silver State Health Insurance Exchange (“Exchange”): Health Plan of Nevada, SilverSummit Health Plan Inc., HMO Colorado Inc. dba HMO Nevada, offering up to 27 plans. The average approved rate increase on the Exchange is 1.6%
“Every year the Division publishes this information in advance so that consumers have an opportunity to preview plans and their rates, said Insurance Commissioner Barbara Richardson. “This is a good time to begin comparing available plans and to visit the new State Exchange website to be better prepared for Open Enrollment.”
Off the Exchange, there are four insurance companies: Health Plan of Nevada, Sierra Health & Life, Hometown Health Plan (HMO company), and Hometown Health Providers (PPO company) offering as many as 33 plans. The average approved rate increase for off-Exchange is 1.9%.
There are several ways consumers can view what their options are before Open Enrollment begins November 1, 2019. For on Exchange plans, the Silver State Health Insurance Exchange, the state agency that connects eligible Nevada residents to qualified health plans through the online marketplace, Nevada Health Link, is excited to announce that Nevada is now a fully operational State Based Exchange (SBE). Nevadans seeking coverage on the Exchange will enroll at NevadaHealthLink.com and not the Federal Health Insurance Marketplace, HealthCare.gov. Consumers who plan on shopping or re-enrolling on Nevada Health Link are encouraged to start their research and planning process early.
Window shopping on the new SBE platform will be available starting Oct. 3rd. Nevada Health Link always encourages consumers to use the free assistance of a licensed enrollment professional or call 1-800-547-2927.
Otherwise, consumers shopping off-exchange can view approved rates and plan information by visiting the Division’s website at www.doi.nv.gov, clicking on “Health Insurance Rates” from the main navigation menu, from the “Health Insurance Rate Review” page, click on “Search for Health Insurance Rates.”
Rates are displayed by age and county and are for non-smokers. The search results are displayed and then sortable by plan name, carrier name, metal tier, and whether the product is offered on or off the Exchange. This allows the search to be limited for quicker focused results.
Because every year there is different market information, consumers are also encouraged to visit the Division’s NV Insurance 101 website at http://insurance101.nv.gov/ to learn more about what health insurance options are available for open enrollment, how to shop for health insurance, and other important topics.
Open Enrollment begins November 1, 2019 and ends December 15, 2019.
I don't know what changes were made to the individual carrier rates in order to nudge the statewide average up by 0.7 points, but it can't have been much. Here's the summary as best as I can figure:
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.