Shocker: Republicans are stingier about helping "deserving" Medicaid enrollees as well!
With Congressional Republicans having clearly decided to target the ACA's Medicaid expansion population for gutting (potentially kicking up to 21 million Americans off their healthcare coverage), they're heavily pushing talking points claiming that they're Deeply Concerned® about preserving Medicaid for those they deem to be "deserving" of coverage:
We acknowledge that we must reform Medicaid so that it is a strong and long-lasting program for years to come. Efficiency and transparency must be prioritized for program beneficiaries, hospitals, and states. We support targeted reforms to improve program integrity, reduce improper payments, and modernize delivery systems to fix flaws in the program that divert resources away from children, seniors, individuals with disabilities, and pregnant women – those who the program was intended to help. However, we cannot and will not support a final reconciliation bill that includes any reduction in Medicaid coverage for vulnerable populations.
As my friend & colleague Andrew Sprung notes:
As I’ve noted previously, the long-established reflex in defending Medicaid is to focus on the most obviously sympathetic populations — medically fragile children, disabled adults, the elderly in long-term care. Focusing exclusively on those groups without centering the expansion population right now plays straight into Republican hands — these are the groups they’re “protecting.” Medicaid advocates need to make it clear exactly who Republicans are selling down the river.
I agree with this 100%. However, since we were on the subject, I decided to take a closer look at just how well Republican-run states are doing on providing coverage to the "more deserving" populations they claim to be wringing their hands over, and discovered to absolutely no surprise whatsoever that they seem to be coming up a bit short on that front as well.
In order to be eligible for tradtional, or non-ACA expansion Medicaid, you generally have to fall into one of several specific categories:
- Pregnant women with low income
- Children in low-income families or in foster care
- People with disabilities
- Seniors with low income
- Parents or caregivers with low incomes
Aside from the disability provision, which is basically folks receiving Supplemental Social Security Income disability benefits (SSI), the categories are generally income-based. However, those income eligibility thresholds vary...and they also vary widely from state to state.
For instance, in my home state of Michigan, children are eligible for Medicaid if their household income is up to 212% of the Federal Poverty Level (FPL), while pregnant women are only eligible up to 195% FPL...and parents of minor children are eligible up to 54% FPL.
If Michigan was a non-expansion state, this would mean that a woman who earns exactly 100% FPL (and whose income remains there for several years) would become eligible for Medicaid if she became pregnant, but once she gave birth, she'd lose eligibility while her newborn child would still be eligible. However, since Michigan has expanded Medicaid under the ACA, she'd still be eligible as well.
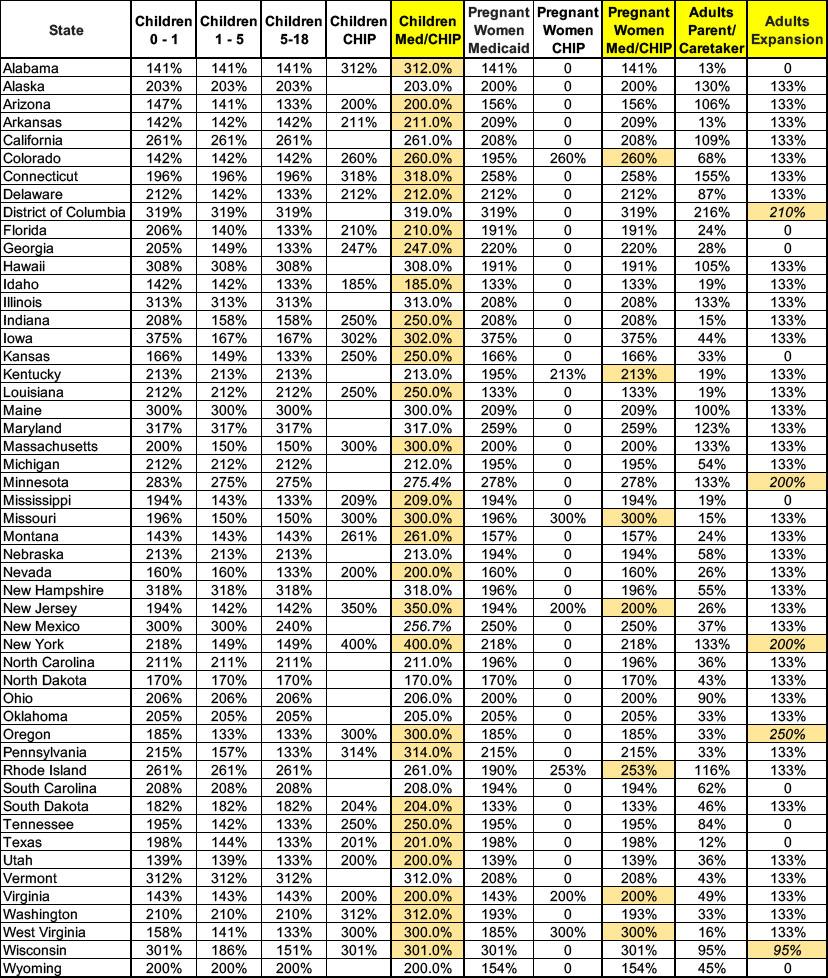
There's actually 8 different income-based eligibility categories: Newborn children up to 1 year old; toddlers age 1 -5; adolescents age 6-18; a separate category for the Children's Health Insurance Program (CHIP) which generally covers children in higher household incomes up to age 19; pregnant women; CHIP for pregnant women; parents & caretakers of minor children; and, for expansion states only, all other adults.
In most states the thresholds for the first 3 categories (children up to 18) are identical, but in a few even these vary, which means a child may go from qualifying to not qualifying from one year to the next even if their parents income remains the same. There's also some other special cases in a few states.
With all this in mind, I've gone through the different categories and averaged the income threshold levels out for each to figure out how generous or stingy each state is when it comes to these populations. I've simplified things by equalizing the child categories & using the highest threshold for CHIP eligibility where available, and did the same thing for the pregnant women category. Doing so looks like this:
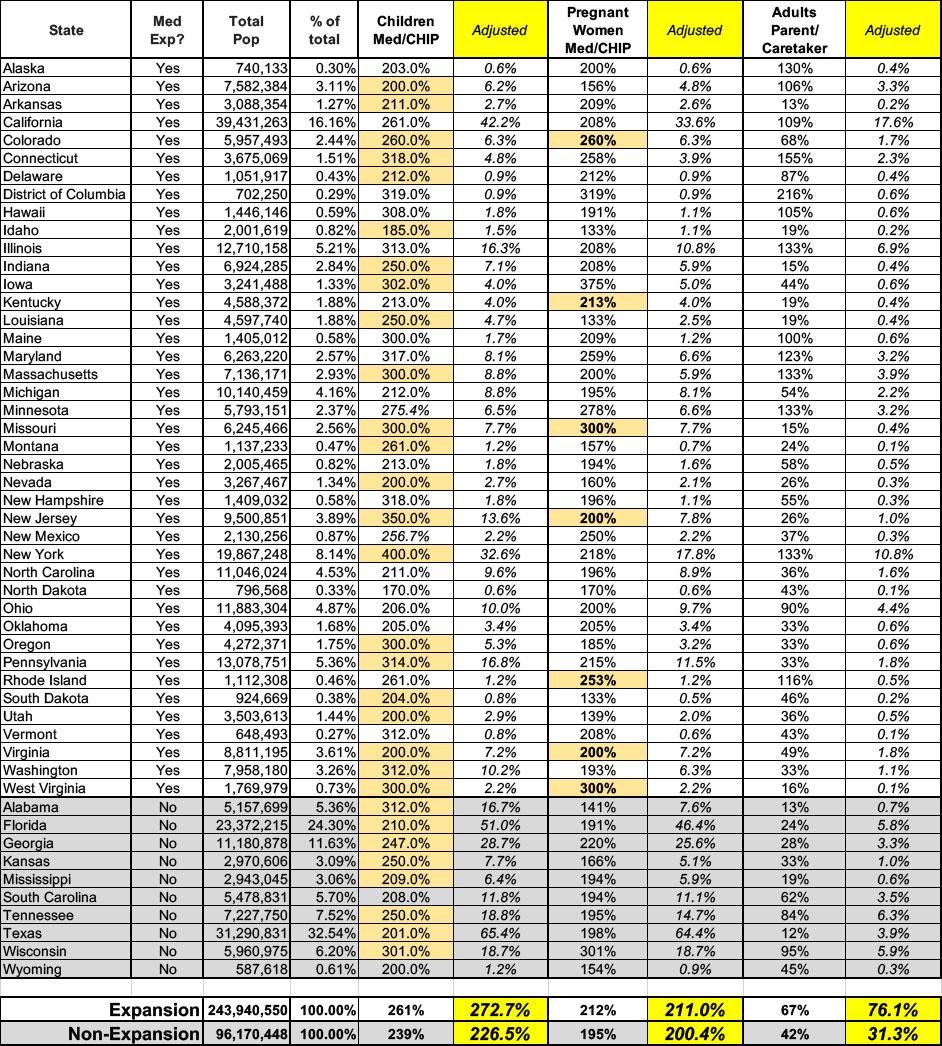
Next, I removed the Adult Expansion column entirely, since the whole point of this is to look at the non-ACA categories, and I had to weight the different states by their population share, since California covering children up to 261% FPL carries a hell of a lot more impact than Wyoming only covering them up to 200% FPL.
I'm grouping the states in two different ways: Expansion vs. non-expansion states, and general Red/Blue/Swing state status.
First, let's look at expansion vs. non-expansion states. In this case, the population weighting is also broken into the two categories, so California makes up 16.2% of the expansion state population while Texas makes up 32.5% of the non-expansion state population.
Doing this looks like so:
The 40 expansion states (+DC), when weighted by population size, provide Medicaid or CHIP coverage to children in households earning up to 273% FPL on average, while the 10 non-expansion states only cover children in households earning up to 227% FPL.
For pregnant women, the expansion states are only slightly higher on weighted average: 211% FPL vs. 200% FPL in non-expansion states.
However, once those women give birth, they and their partners are significantly better off in expansion states (76% FPL) than in non-expansion states (just 31% FPL)...and in fact that 76% threshold is irrelevant in expansion states since they're actually covered up to 138% FPL via the ACA.
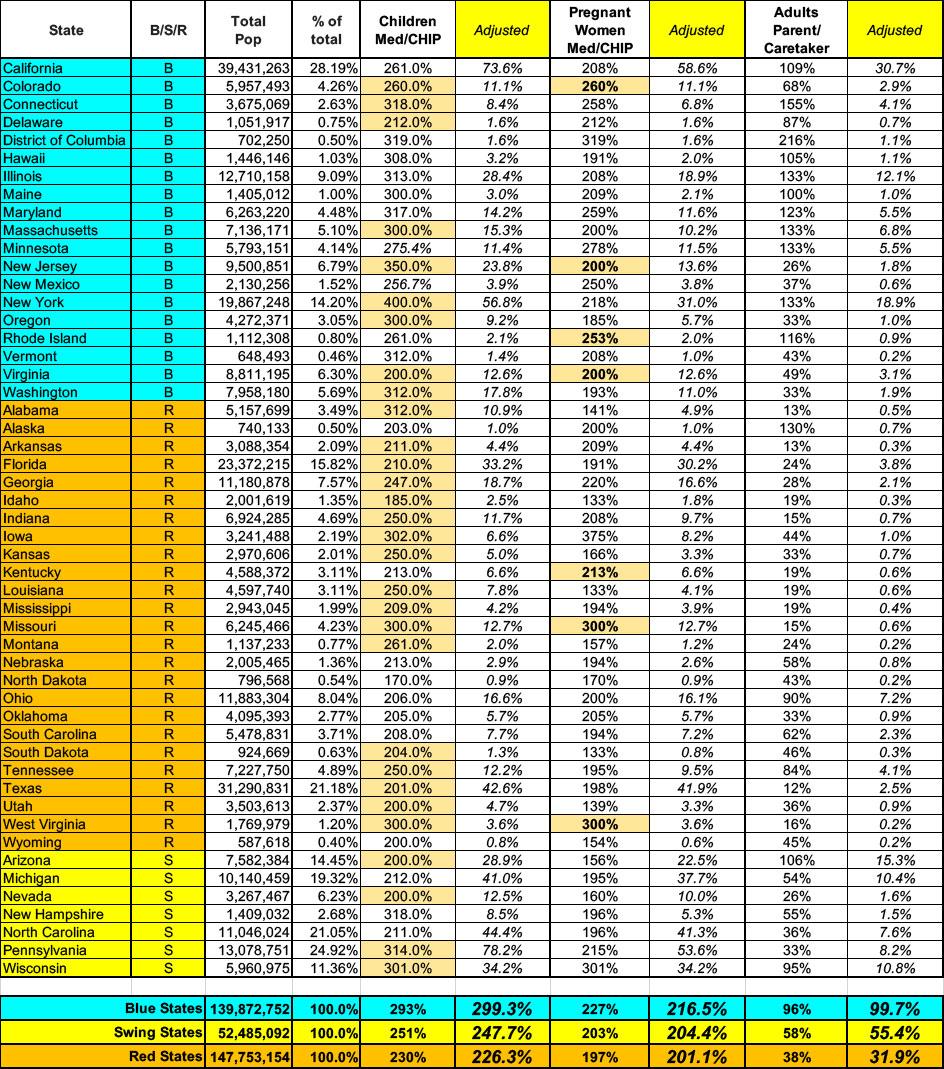
The only problem with this logic is that there's a lot of clearly red states which have expanded Medicaid under the ACA, although many did so via statewide ballot initiative over the objections of their Republican governors and/or legislatures: Utah, Nebraska, Missouri, Oklahoma & South Dakota, to name a few.
Therefore, I've also run the same calculations with the states broken into three groups: Blue, Red and Swing States. It's important to note that "Swing State" isn't necessarily the same here as it is for Presidential elections. Georgia, for instance, is considered a swing state for Presidential races, but from a state government POV it's clearly solid red. Kansas may have a Democratic governor, but is also clearly red; conversely, Vermont's governor may technically be a Republican but you'd be laughed at if you said VT was a "swing state."
With that in mind, here's how the spreadsheet looks when the states are broken out this way:
Looked at this way, blue states, on weighted average, cover children up to 299% FPL; pregnant women up to 217% and parents/caretakers up to 100% (actually 138% FPL since every blue state has expanded the program).
By contrast, red states only cover children up to 226% FPL, pregnant women up to 201% and parents/caretakers up to 32% FPL on weighted average.
In all three categories, the swing states are appropriately sandwiched in between at 248%, 204% and 55% respectively.
I realize that there are some caveats in my methodology which make it more complicated than this, but the larger point is valid: If Republicans are serious about making sure that the "vulnerable" populations have Medicaid/CHIP coverage, perhaps they should bump up the thresholds those groups are eligible for to at least the same levels as the blue states for starters.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.