ACA Navigators: Using Seema Verma's own logic, she saved $53 million to screw several hundred thousand people.
Here's an overview of the ACA's "Navigator" and "Certified Application Counselor (CAC)" programs:
Navigators
Navigators play a vital role in helping consumers prepare applications to establish eligibility and enroll in coverage through the Marketplaces and potentially qualify for an insurance affordability programs. They also provide outreach and education to raise awareness about the Marketplace, and refer consumers to health insurance ombudsman and consumer assistance programs when necessary. Navigators are funded through federal grant funds and must complete comprehensive federal Navigator training, criminal background checks, and state training and registration (when applicable), prior to assisting consumers.
Certified Application Counselors (CACs)
Certified application counselor designated organizations (CDOs) are a vital component of the assister community. In the Federally-facilitated Marketplaces (FFMs), CDOs oversee certified application counselors (CACs) who are trained and able to help consumers seeking health insurance coverage options through an FFM. Organizations that wish to become CDOs designated by the Centers for Medicare & Medicaid Services (CMS) to serve in an FFM must submit an online application and enter into an agreement with CMS. These groups might include community health centers or other health care providers, hospitals, or social service agencies.
Back in the August 2017, the Trump Administration decided to slash the marketing/outreach advertising budget for HealthCare.Gov by 90%, from $100 million down to just $10 million/year. Much has been written about this by myself and others, so I won't go too deeply into that again here.
At the same time, however, the Trump Administration also decided to slash the ACA's Navigator program by 39% that year as well...and further yet the following year.
Trump's CMS Administrator Seema Verma tried to justify the massive slash in funding by claiming that the Navigator grant program was extremely wasteful and inefficient, and cherry-picked data regarding enrollment in private marketplace plans as their only benchmark for how "efficient" or "effective" Navigators and CACs were:
CMS presented several reasons in explaining the reduced funding for Navigators...citing data it collects from healthcare.gov, CMS argues that Navigators have played a limited role in facilitating enrollment in the marketplaces, particularly compared to brokers.
The problem with this should be obvious:
Navigators and brokers do not serve the same populations or provide the same services. According to findings from the KFF Marketplace Assister Survey, while the work of brokers overlapped to a significant extent with that of Navigators and other marketplace assister programs, these professionals were not interchangeable. Brokers were significantly less likely than Navigators to help individuals who were uninsured, had limited English proficiency, or who lacked internet at home (Figure 2). Brokers were also far less likely to help complete applications for Medicaid or CHIP for low-income consumers who learn through the “no wrong door” marketplace application process that they are not eligible for premium tax credits but may be eligible for public plan coverage.
I haven't written much about the Navigator/CAC program in awhile, but the other day, Ben D'Avanzo brought something interesting to my attention:
Last night HHS quietly released data about ACA Navigators. Imagine how many people could have gotten covered if they didn't slash the program? pic.twitter.com/13YjZbRluq
— Ben D'Avanzo (@BenDAvanzo) January 20, 2021
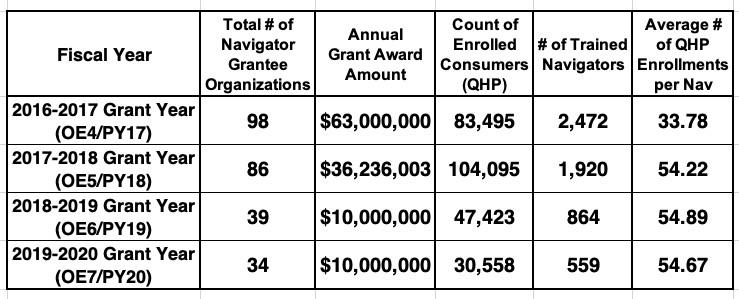
This is what he was referring to...an excel spreadsheet summarizing the Navigator program funding and related enrollment data from 2016 - 2020. Interestingly, there's no accompanying cover letter or press release or anything...just the spreadsheet itself. Huh.
It does include some data collection & methodology notes at the front:
QHP Data (Count of Enrolled Consumers): This data is pulled from applications submitted to the Marketplace via Healthcare.gov on which a Navigator’s unique ID number was included. This data is subject to certain limitations. In particular, the the data does not encapsulate Navigator-assisted QHP enrollments in which a Navigator's unique ID number was not included on an application, or was incorrectly entered on an application. In addition, prior to the 2018-2019 period, consumers were only able to identify one entity's identification number on the same application, which did not allow for multiple navigators and agents or agents or brokers to include their identification. The data also does not reflect coverage effectuations or plan cancellations that may occur throughout a given year, but instead is static for the week that the consumer's application was submitted to the Marketplace with a plan selection. As a result, the "totals" for each grant year are a cumulative total of all the weeks in a respective grant year.
That's...a lot of pretty important caveats.
Medicaid/CHIP Enrollments: Navigator assistance in enrolling in Medicaid/CHIP (level of Navigator assistance varies by state)
Post-Enrollment Assistance: Navigator assistance provided on one of the following post-enrollment topics: Marketplace tax forms, filing Marketpl nace exemptions, submitting Marketplace or insurance coverage appeals, resolving DMI, determining SEP eligibility, resolving APTC/CSR issues, or answering questions regarding ESC
Health Insurance Assistance and Literacy: Responding to general inquiries from consumers, educating consumers on health insurance literacy (including how to use their insurance, make premium payments, locate providers, and resolve billing/payment issues with their issuer)
Referrals to Other Health Insurance Providers: Referrals made by a Navigator to another entity, either at the request of the consumer or because the consumer's issue requires assistance outside of the Navigator's training. Referrals made to the following are captured here: A/B, state Medicare office, Other Consumer Assistance/health insurance program, State DOI, Issuer of consumer's plan
For 2020, the spreadsheet changes a couple of the columns and descriptions. Instead of "Health Insurance Assistance & Literacy" they refer to "Total 1:1 Consumer Assistance", and "Post-Enrollment Assistance" is listed as "Optional".
All 1:1 assistance provided to consumers by Navigators, excluding QHP enrollments and Medicaid/CHIP enrollments or referrals. Assistance in this category includes activities such as: responding to general inquiries from consumers, educating consumers on health insurance literacy (including how to use their insurance, make premium payments, locate providers, and resolve billing/payment issues with their issuer), making referrals to another entity (either at the request of the consumer, or because the consumer's issue requires assistance outside of the Navigator's training). Referrals made to the following are reported by Navigators: A/B, state Medicare office, Other Consumer Assistance/health insurance program, State DOI, Issuer of consumer's plan.
Regulatory changes finalized in the 2019 Payment Notice made assistance by Navigators with post-enrollment activities permissible, but no longer required. Although these activities are no longer a required Navigator function, Navigator grantees continue to assist consumers with a variety of post-enrollment topics. To align with the regulatory changes, reporting on these activities is now optional as well.
Navigator assistance provided on one of the following post-enrollment topics: Marketplace tax forms, filing Marketplace exemptions, submitting Marketplace or insurance coverage appeals, resolving DMI, determining SEP eligibility, resolving APTC/CSR issues, or answering questions regarding ESC
OK, with all that out of the way, let's see the data!
The summary tables at the top appear to kind of, sort of support Verma's point:
If you stop with the summary tables, it certainly looks like Verma kind of has a point: For 16% of the cost, they were still able to enroll 37% as many people! What a bargain! And look at that--the "efficiency level" jumped by 62%, with each navigator enrolling 55 people for 2020 vs. 34 apiece in 2017!
Except, of course, for a few problems with this logic: The primary goal of the Navigator program isn't to "save taxpayer money" but to "help as many people as possible enroll in and utilize healthcare coverage." On that front, it looks like slashing the budget from $63 million to $10 million resulted in 53,000 fewer people not getting covered last year.
But wait, there's more!
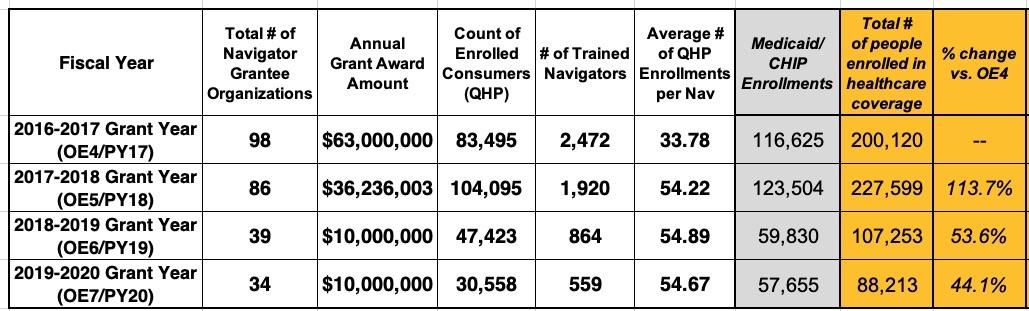
It's quite telling that the annual summary tables leave out several important columns found in the grantee-level breakout below them, which include the columns defined above, along with another critical one: Total Medicaid/CHIP Enrollments.
Let's see what happens when we add those to the mix:
Hey, look at that! The total number of actual human beings who ACA Navigators helped enroll in healthcare coverage of one type or another dropped from over 200,000 in 2016 to just 88,000 in 2020...a 56% reduction. On a percentage basis this is actually better than QHP enrollment alone, but it stll means 112,000 fewer people getting help enrolling last year, thanks in large part to the reduced Navigator budget.
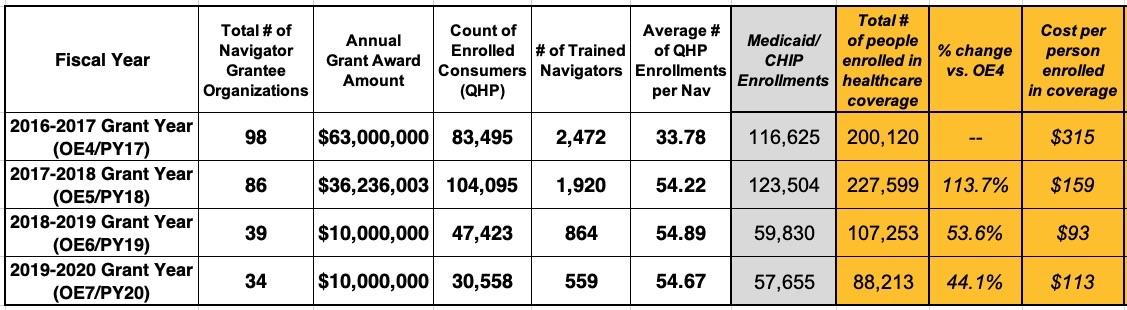
Now, if you stop here, I suppose you could still argue that Verma had a point regarding the Navigator funds being used "inefficiently", since you're still seeing 44% as many enrollees for 16% of the cost.
However, by that same logic, it seems to follow that keeping the total budget the same while still making the other structural changes in HOW the funding was used should have resulted in getting a lot more people enrolled, shouldn't it? After all, using Verma's own "efficiency" measurement benchmark, it costs 30% as much to enroll each person into an ACA policy (or Medicaid) under her system than it did under the Obama-era system, right?
Using her own logic, increasing the Navigator program budget back from $10 million to $63 million while keeping all the other changes she made the same should result in at least 6.3x as many people being assisted, right? That'd be around 555,000 people total instead of the 88,000 assisted last year (467,000 more people). Alternately, you could argue that since she claims to have reduced the cost per enrollee by 70%, that means that increasing the budget 6-fold should result in a 3.3x enrollment increase, or 294,000 (206,000 more people).
Of course, neither of these arguments make a lot of sense when you take into account all of the other factors at play (especially the fact that Navigators also do a lot more than simply get people enrolled, and a lot of that additional assistance can't be measured easily on a spreadsheet)...but I'm trying to follow Verma's "efficiency" argument here.
Regardless of how you look at the numbers, the fact that Seema Verma--the same woman who never met a Medicaid work requirement she didn't love--decided to pretend that Medicaid enrollees aren't even worth counting as people, is pretty telling.
Anyway, I sincerely hope that once Biden's new HHS Dept. and CMS Administrator are squared away, they'll make sure to reinvigorate and restore the budget to the Navigator/CAC program going forward.