New This Fall: ACA exchange plans will include "Quality Ratings"
(OK, no, this does not appear to be a "Yelp!"-like system where enrollees can directly influence the star ratings...I just posted the logo for the hell of it)
I didn't catch this when the press release went out a few days ago, but this could be significant...or it could be a big batch of nothing:
CMS is Bringing Health Plan Quality Ratings to All Exchanges for the First Time
Consumers will have improved access to health plan quality information for the 2020 Open Enrollment PeriodFor the first time, the Centers for Medicare & Medicaid Services (CMS) will require the display of the five-star Quality Rating System (or star ratings) available nationwide for health plans offered on the Health Insurance Exchanges beginning with the 2020 Open Enrollment Period. This step builds on the Trump Administration’s overall commitment to increasing transparency and empowering consumers to make informed healthcare decisions for themselves and their families. Beginning with this year’s Open Enrollment Period, consumers will be able to compare health coverage choices using a five-star quality rating of each plan on Exchange websites, including HealthCare.gov, similar to other CMS star rating programs, such as the easy to understand Nursing Home Compare website and Medicare Advantage.
...Under the five-star Quality Rating System, Exchange health plans are given a rating on a 1 to 5 scale, with 5 stars representing highest quality. Star ratings are based on a number of important factors, including how other enrollees rate the doctors in the plan’s network and the care they receive, how well the plan’s network providers coordinate with enrollees and other doctors to give members healthcare that achieves the best results, and the overall administration of the plan including customer service and availability of information. In some cases — like when plans are new or have low enrollment — star ratings may not be available in all areas of the country. The lack of a star rating does not mean the plans have a low quality rating.
The overall star rating is based on three categories: Medical Care, Member Experience and Plan Administration. Medical Care is based on how well the plans’ network providers manage member healthcare, including providing regular screenings, vaccines, and other basic health services. Member Experience is based on surveys of member satisfaction with their healthcare and doctors and ease of getting appointments and services. Plan Administration is based on how well the plan is run, including customer service, access to needed information and network providers ordering appropriate tests and treatment.
During the 2017 and 2018 Open Enrollment periods, CMS conducted a limited pilot and displayed star ratings on HealthCare.gov in two states, Virginia and Wisconsin. The pilot was expanded to include three additional Exchange states – Michigan, Montana, and New Hampshire – during the 2019 Open Enrollment period. The display of Star ratings will now be expanded to every state during the upcoming Open Enrollment period making it available to consumers around the country this fall.
As part of today’s announcement, CMS is posting star ratings and quality measure level data from the 2019 Plan Year in a Public Use File (PUF). The agency is making this data from last year available to the public, researchers, agents, brokers, states, health issuers, and consumer groups to allow them to use and analyze the data. The star ratings data for the 2020 Plan Year will be released closer to Open Enrollment.
One of CMS’s primary goals is to offer Americans who choose to enroll in the Exchanges the best consumer experience possible. Displaying health plan quality information makes it easier for consumers to pick a plan that best meets their needs. CMS is also further advancing its commitment to improve the accuracy and value of the information available to consumers and promoting quality improvement in the healthcare industry.
The 2020 Open Enrollment Period is November 1, 2019 to December 15, 2019.
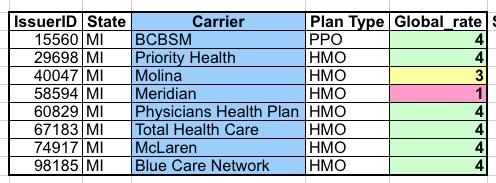
I downloaded the PUF for 2019 and took a look at the Michigan carriers listed. It's extremely cryptic and wonky, and I had to do some research to look up the actual carrier names since they aren't included in the CSV file itself, but as far as I can tell, here's what it looks like here in my home state:
Unless I'm misinterpreting the spreadsheet, it looks like of the 10 carriers participating in the ACA exchange this year, eight of them have star ratings listed. Of those, six received 4 starts, while one (Molina) received a middling grade of 3 and one (Meridian) received a crappy 1 star rating. Two other carriers don't have ratings at all (Alliance and Oscar). There's also an 11th carrier, Health Alliance Plan, but they're only selling individual market policies off-exchange so don't get a rating.
Will this have any noticeable impact on enrollment, market share or quality of service...or will people just ignore the ratings altogether? Who knows? My guess is that it will have some negative impact on Meridian, for instance, that any carrier with a 3 or better rating probably won't notice any difference at all.