Here's how even the Trump Administration's "insignificant" lies can lead to major policy sabotage down the line
If you've followed this site for awhile, you may recall that about a year ago, I called out the Centers for Medicare & Medicaid (CMS) for trying to pull a fast one regarding the 2017 Open Enrollment Period data.
The short version is that they tried to make it look as though only 10.3 million of the 12.2 million people who selected Qualified Health Plans (QHPs) from the ACA exchanges actually paid their first month's premium and were actually enrolled (i.e., "effectuated"), or around 84%. They then tried using this "fact" as evidence of how the ACA was failing, etc etc, because this was supposedly down from 2016 levels.
The difference, as I noted at the time, is that the 2016 effectuation numbers were as of March, while the 2017 effectuation numbers were as of February. This made a big difference, because around 500,000 people who enrolled during 2017 Open Enrollment couldn't have been effectuated for February...because about half a million people enrolled between Jan. 16th - Jan. 31st, which meant their policies weren't even scheduled to begin until March.
At the time I assumed CMS was only doing this as yet another way to bash Obamacare (which would have been bad enough, seeing how the ACA is the law of the land, which means CMS isn't supposed to be expending resources to trash it using taxpayer funding).
However, it turned out to be bigger than that.
CMS just released this year's effectuation report, and the good news is that it actually includes quite a bit of useful data, which I dug into last week in a four-part analysis. My very first entry noted that CMS was once again playing fast and loose with the enrollment data, in a slightly different way. This time around, they claimed that thanks to the amazing work of the Trump Administration (no comment), they had somehow managed to improve the effectuation rates dramatically:
As of March 15, 2018, 10.6 million individuals had effectuated coverage through the Federal and State-Based Exchanges for February 2018, meaning that they selected a plan, paid their first month’s premium, if applicable, and had coverage in February 2018. The total number of members with February 2018 coverage is about 9 percent lower than the number of individuals (11.8 million) who made plan selections during the 2018 Open Enrollment period, as reported in the 2018 Open Enrollment Final Report released by CMS in early April. The number of individuals with effectuated coverage for February 2018 is approximately 3 percent higher than February 2017 effectuated enrollment of 10.3 million individuals, as of March 15, 2017.
This immediately caught my eye:
As I noted last summer:
How much of a difference does that make? Well, according to my spreadsheet, as of 1/15/17, around 11,719,286 people had signed up for an exchange policy.
That means that if I'm reading the CMS press release correctly (and I admit the wording of it is a bit confusing...deliberately, I suspect), that means that instead of dividing 10,330,759 numerator into the full 12,216,003 denominator, it should only be divided into 11,719,286.
Assuming I'm reading the CMS report correctly, that means that as of 3/15/17, 88.2% of January and February enrollees had paid their first monthly premium. That's a net drop of only 11.8%, a couple of points better than prior years.
Again, that's 11.8%, not 15%.
Yes, the 2018 effectuation rate is indeed slightly better than it was last year as a percentage of those who select plans, but not much: It was 90.6% vs. 88.2%, which isn't worth getting too excited about.
But it's actually more than that, because for 2018, the Open Enrollment Period deadline was cut in half, back to December 15th. This means that instead of 96% of all QHP selections being effectuated in time to be counted in February, over 99.5% of those who chose plans were, with only a relatively small number signing up after January 15th in California, New York, DC and Massachusetts. In other words, the February rate was front-loaded to give a false impression of an improved effectuation rate.
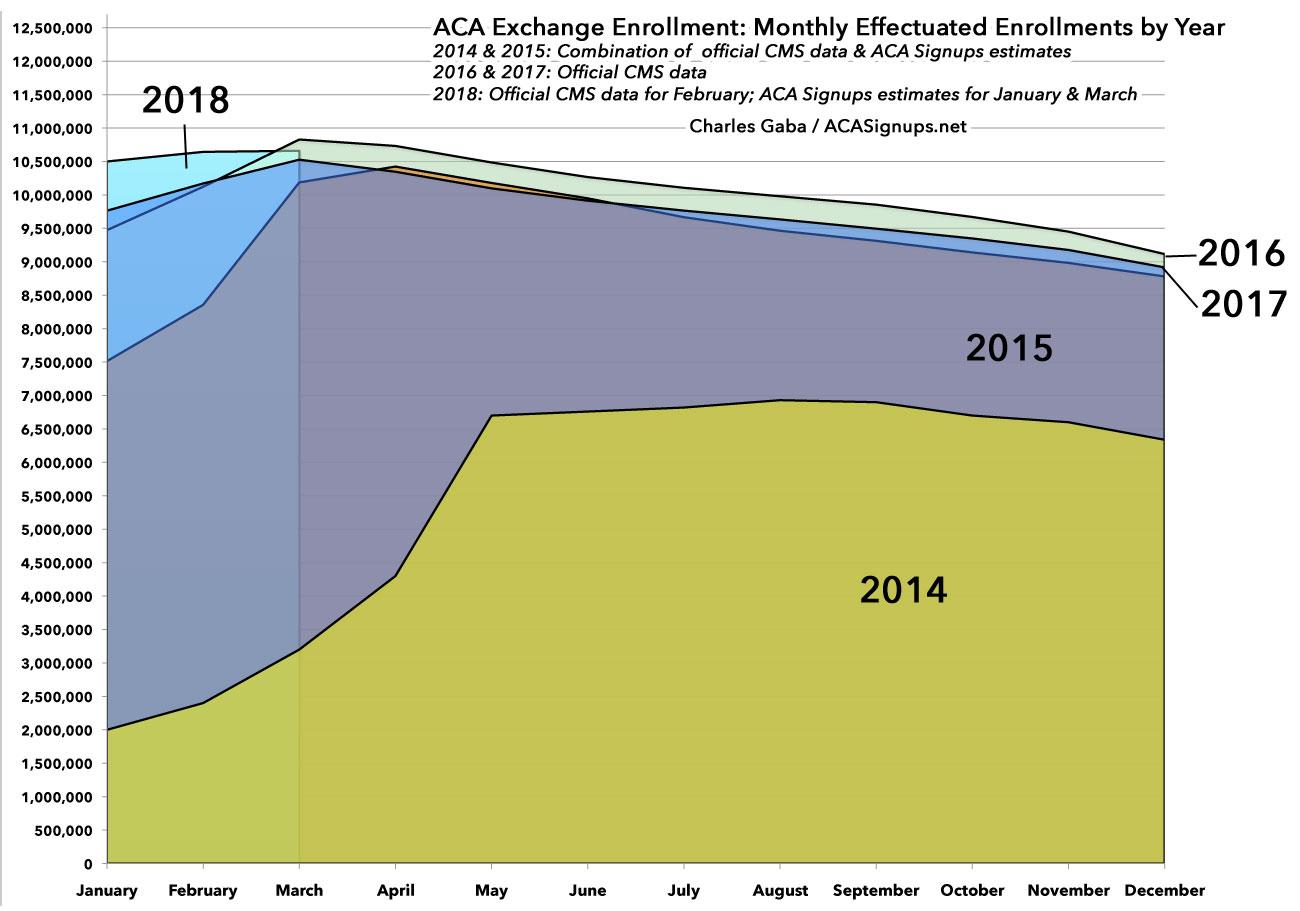
Here's what the monthly effectuations look like over the full 12-month period for every Open Enrollment Period so far, including the first quarter of 2018:
As you can see, unless there's a dramatic change in attrition/retention patterns over the rest of 2018, the odds are extremely high that December 2018 effectuations will be very similar to what they were in 2015, 2016 and 2017.
Don't get me wrong, it's not a bad thing to have more people enrolled starting earlier in the year; the whole idea behind the ACA is for as many people as possible to have year-round coverage. However, the fact remains that in 2017, the Trump Administration fudged the numbers to make it look like Obamacare Sux. In 2018, they fudged the numbers to make it look like Trumpcare Rox thanks to all the amazing innovative ideas CMS Administrator Seema Verma came up with, like slashing the enrollment period in half, slashing the HealthCare.Gov marketing budget by 90%, slashing the navigator/outreach budget by 40% and so on.
But it gets worse, because yesterday, Trump's CMS announced that they're going to slash the 2019 navigator/outreach budget even more drastically, from $36 million to just $10 million.
And here's where I need to give Andrew Sprung (aka Xpostfactoid) props for catching this tidbit in CMS's justification for the cuts:
To justify gutting funding for the navigators who help low income people enroll in health insurance subsidized by the ACA (Medicaid as well as marketplace), CMS is turning a bogus talking point it concocted last year inside out. Here's the current claim, as reported by KHN's Phil Galewitz:
CMS also notes that after last year’s navigator funding was reduced, the overall enrollment in Obamacare plans increased slightly (when counting people who paid their first month’s premiums) to 10.6 million people.
Sprung picked up my ball and ran with it, crunching the numbers, correcting for the end dates and starting effectuation dates for each year, and notes that:
If those enrollees effectuated coverage at the same rate as enrollees before 1/15 (88.5%), there were 10.8 million who had effectuated or would soon effectuate as of the time of CMS's tally. That total outstrips this year's.
In other words, in an apples-to-apples comparison, instead of 10.6 million (2017) vs. 10.3 million (2016), it would actually be more like 10.6 million vs. 10.8 million.
As Sprung notes, this may not seem like a big deal, but...
But in another sense, it matters a lot. The Trump administration did everything it could to depress admission this year: radically cut advertising as well as enrollment assistance; denigrate ACA programs and (via Trump himself) declare them dead; keep insurers in suspense over Cost Sharing Reduction (CSR) reimbursement, then cut it off -- all while a Republican Congress came within a whisker of repeal. As it turned out, the most egregious act of sabotage -- the CSR funding cutoff -- had a paradoxical though long-predicted effect, as priced-in CSR, concentrated in silver plans, created large discounts for subsidized buyers in bronze and gold plans...About 2 million enrollees took advantage of those discounts, which likely increased enrollment by several hundred thousand, partly offsetting the effects of sabotage efforts that included the prior round of cuts to navigator funding.
CMS is thus effectively using the "CSR backfire" to justify cutting federal funding for navigators to a negligible $10 million -- down from $36 million last year and $63 million the year prior -- which will hurt low income prospective enrollees. At the same time, they're repurposing last year's lowballing of effectuated enrollment through February to take credit for the relatively good 2018 enrollment totals they did everything in their power to depress -- touting 2018 as "our most cost effective and successful open enrollment to date." That's governance under Trump.