Here's the future of Medicaid expansion under "work requirements".
This morning I was contacted on Twitter by a woman in Louisville, Kentucky who appears to be in pretty dire straits:
On 7/1/18, in Ky, my Medicaid/ ACA will be canceled. I may still need a brain shunt, LP #8, RXs, PT, etc. I was informed that my PCP could write a letter stating I was "Medically Fragile" but even then the provider has final say. Like fox guarding hen house. Please help me/DM
Here's her story according to her GoFundMe page (I've cleaned up the formatting a bit for easier readability):
I am a disabled attorney living with my 76-year-old mother who takes care of me. In 2011, I was bitten by a tick and was infected with Ehrlichiosis Chaffeensis and Rickettsia. A week later, I contracted Coxsackie B4 virus. Because I was kept on antibiotics for 19 years, I had no immune system to fight these illnesses.
I was untreated by my FORMER doctor for 11 mos. By then, the tick bacteria had infected my Cerebral Spinal Fluid. Now I have a Pseudotumor Cerebri and have lost the use of my left side. (Coxsackie virus is a "Cousin" of Polio). I cannot drive. I need help dressing/bathing. I just had my 7th spinal tap on Monday last. I may need a brain shunt to drain the excess fluid. I have been hospitalized at least 5 times, have been to the Mayo Clinic, have had 20 + MRIs/CT scans, and have been rushed to the ER at least 20 times. I live in Chronic Pain.
One of my Ten + medicines cost $1600/mo. Before the ACA, I paid $1000/mo. + meds for my health insurance. I quickly went through both my mine and my mother's LIFE SAVINGS of over $120,000. Three months after I was sworn in as an attorney, my father was diagnosed with terminal cancer and given six mos. to live. I closed my law office and moved back home to care for him. He made it almost 2 years. My parents had been married 40 years. My mother and I already lost my brother to a hit and run driver. He was 19 and I was 14. My mother cannot bear to lose her only other child. We are about to lose our home of 47 yrs. Besides being homeless, our home is the last thing we have left of my Dad and brother.
I also face losing my healthcare under the ACA. I tried to do everything "right". I went to school to take care of my parents and worked as a criminal defense attorney helping those less fortunate and the wrongfully charged and convicted. During my undergraduate years I ran a childcare program that cared for low-income and disabled children. We had no life insurance when my dad died. He accidently let it lapse and was too embarrassed to tell us.
My mother worked until age 75 but had to quit to take me to my Drs. appointments. If we don't lose our house in the next six mos., I will be homeless when she dies. I can't drive. My disability process takes 24 mos. We cannot make it that long. If I lose my Healthcare, she will have to try to find a job at age 76. Even if I am able to keep my ACA, we will lose our family home. Please, will someone help us? If she outlives me, she will be homeless with no money for retirement or medical assistance. If someone can help us, I promise to pay it forward. I will take in rescue animals or take in a person who needs shelter. We are desperate and need help. Please open your hearts so that we can keep our home. I am in chronic pain and my mom and I want to die at home like my father.
God bless you, Julie
I contacted Julie privately and she gave me a bit more detail about her situation...especially as it pertains to her enrollment in Medicaid, which appears to only be possible thanks to ACA expansion:
Me: I take it you’re among those who’ll be subject to the new work requirement rules?
Julie: Yes. My Dr. already wrote me a letter stating I could do no meaningful work. Now, I've received notice that my Medicaid/ ACA will be canceled as of 7/1/18. My Dr has to write another letter stating I am "Medically Fragile". My disability is still pending. Once I get this new letter, it is my understanding that the final decision will still be left up to the Ins. Cos. Talk abt the fox guarding the hen house.
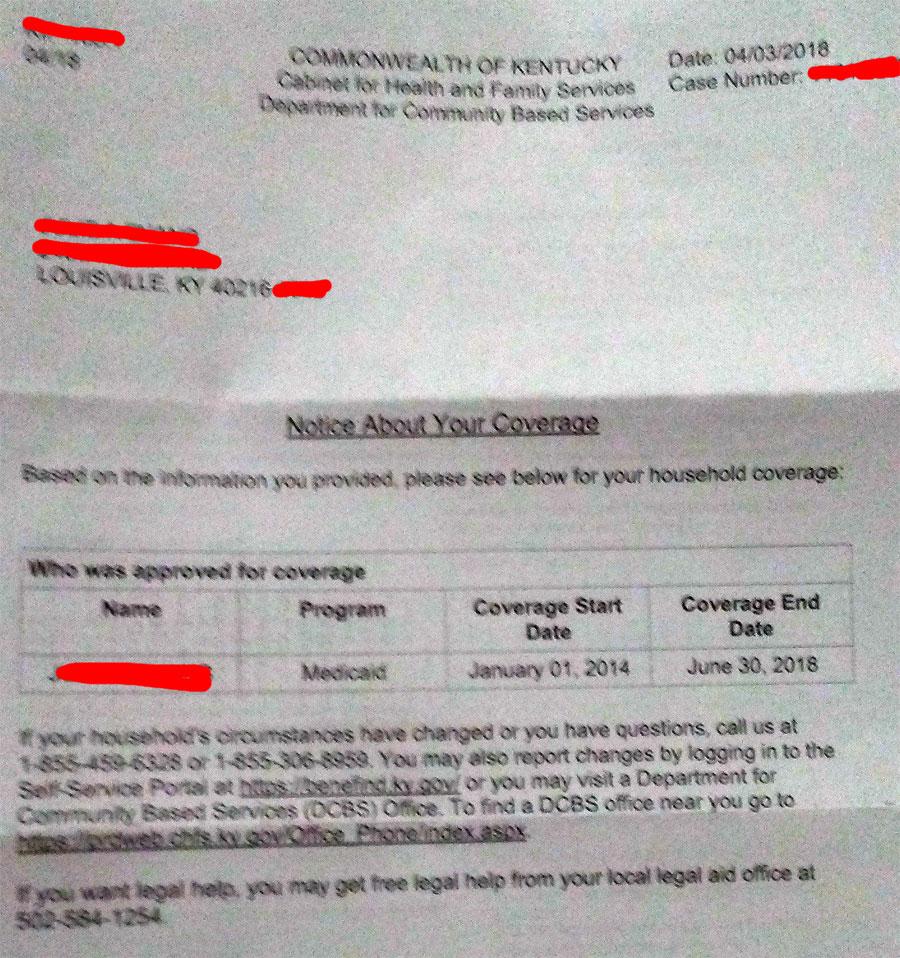
Here's the letter [screen shot below] notifying that my Medicaid/ ACA will be canceled on 7/1/18.
For the work requirement I was able to get my PCP to write a letter, stating that I was too ill to work. I had my SSI/SSDI hearing & the judge ruled in my favor for SSI (I had waited too long for SSDI bc I kept thinking I would get better & be able to go back to work: I was a trial attorney) . But it could take 3-4 mos to go through bc of the red tape. So, once again, I fell through a crack. I have had to set up a gofundme account to pay for my RX, food, & shelter. I live in Louisville which has always been a blue city & we haven't had a GOP gov. for years! I can't afford to move bc we are underwater on our mortgage & my mom is 76. If I am declared " Medically Fragile " will they still come after me?
Now, I want to be clear about something: I have not independently confirmed Ms. Evans' story beyond her words and the screenshot of her Medicaid termination shown above. Is it possible that parts of her story are exaggerated or made up? Anything's possible.
However, that's not the point. The point is that even if her particular story doesn't end up panning out, there are thousands of other people faced with similar situations who will be extremely hard-pressed to be able to meet the "work requirement" provisions for Medicaid coverage being laid out in Kentucky and other states.
UPDATE: Strike that...I have received enough confirmation of Ms. Evans' story to be reasonably confident that her entire awful story is accurate.
On top of everything else,
Several commenters noted that the state's Medicaid offices, where many beneficiaries must go to report those changes, and the phone lines used to call to report changes are already busy and the calls and visits are time consuming. We understand that the state has made improvements in its call center operations and beneficiaries are able to report changes both over the phone and electronically. This is expected to reduce the burden of reporting and increase beneficiaries' likelihood for success in meeting the requirements. CMS also will track beneficiary success in meeting these requirements as part of ongoing demonstration monitoring.
The "good" news is that...
Additionally, Kentucky will allow good cause exemptions in certain circumstances for beneficiaries who cannot meet their requirement. Kentucky also will be required to provide reasonable modifications for beneficiaries with disabilities.
...but again, that assumes that there are "reasonable" people making such decisions who aren't incredibly overloaded and backed up.
As commenter "HeyMikey" noted over at Daily Kos earlier today:
An often overlooked, but real, reason to vote against Medicaid work requirements: the bureaucracy can’t or won’t administer them correctly. I’ve heard this same story over and over again from people on SNAP (food stamps) here in Georgia:
You have to “recertify” by providing all your verification paperwork every 6 months. The only way you are allowed to submit the paperwork is by uploading it to the DFACS website. The DFACS website gives you no tracking number, no confirmation number, no way you can verify what you submitted and when. But you upload all your paperwork and assume everything is fine.
A few weeks later you’re checking out at the grocery on the day after your SNAP is credited to your account each month, and the cashier tells you there’s no credit on your EBT (Electronic Benefits Transfer, SNAP) card. You go home (hungry), call the DFACS statewide 800 line to see what paperwork they didn’t get—copy of your driver’s license? Your latest pay stub? Your third child’s birth certificate?—and you’re on hold for HOURS. Like, 8 hours. (Seriously.) The state just doesn’t give DFACS enough money to hire enough operators to handle the call volume.
A few days, maybe a couple weeks later, a notice comes in the mail from DFACS. It says you’ve been cut off because you didn’t submit all the required paperwork. It still doesn’t tell you which paperwork they need that they don’t have. It tells you to call the 800 line. You do, again you’re on hold for hours, still nobody answers.
Eventually you give up with the calls, and you walk into your local DFACS office. They tell you, “We can’t discuss that with you here. You have to call the statewide 800 number.”
You have the right to appeal, but nobody knows that, and the caseworkers will steer you into just filing a new application. Which takes weeks or months. You never get back the SNAP benefits you lost in the interim.
Apply that system to Medicaid work requirements, and you have people dying.