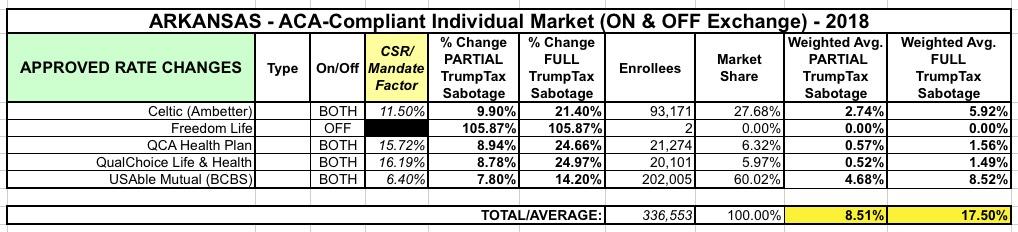
Arkansas: Approved rate hikes: 8.5% with CSR payments, 17.5% without them
Now that we've passed the 9/27 contract signing deadline for 2018 carrier participation on the ACA exchanges, the state insurance departments are posting their approved final rates pretty quickly. Arkansas has done a fantastic job of clearly laying out not just what the rate changes will be, but is explicitly stating how much of those increases are due to the GOP's refusal to formally appropriate CSR reimbursement payments next year:
Insurance companies offering individual and small group health insurance plans are required to file proposed rates with the Arkansas Insurance Department for review and approval before plans can be sold to consumers. The Department reviews rates to ensure that the plans are priced appropriately. Under Arkansas Law (Ark. Code Ann. § 23-79-110), the Commissioner shall disapprove a rate filing if he/she finds that the rate is not actuarially sound, is excessive, is inadequate, or is unfairly discriminatory. The Department relies on outside actuarial analysis by a member of the American Academy of Actuaries to help determine whether a rate filing is sound.
Below, you can review information on rate filings for Plan Year 2018 individual and small group products that comply with the reforms of the Affordable Care Act. You may also view rate filings for previous years through the federal government's Rate Review website here.
Users will only be able to view the public details of the filing, as certain portions are deemed confidential by law (Ark. Code Ann. § 23-61-103).
Note: Companies offering on-marketplace plans were allowed to make an alternative filing on August 21 pursuant to AID Bulletin 14-2017.
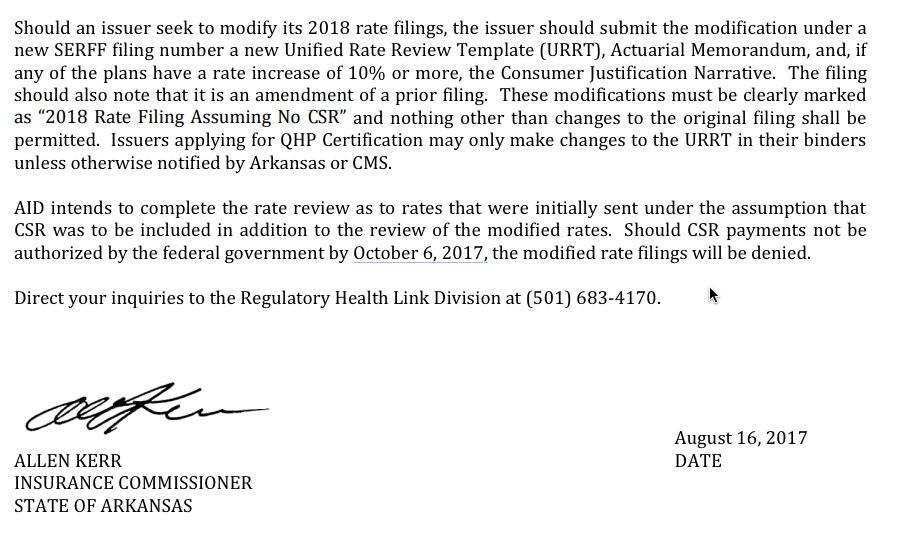
The bulletin in question states that the Arkansas Insurance Commissioner hopes to use the lower rate filings (which assume CSRs will be paid), but if they don't receive formal appropriation by October 6th, they're gonna have to use the "no CSR" rates, which are an additional 9 percentage points higher:
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.