Exactly which no-cost services did hack judge O'Connor strike down? It's complicated.

My ongoing Braidwood v. Becerra post has grown so long and has had so many updates that it was becoming unwieldy, so I started a new post.
Kaiser Family Foundation Vice President Cynthia Cox posted a thread on Twitter yesterday which gives an brief overview of which of the preventative services required to be covered at no cost to the enrollee by the Affordable Care Act are actually threatened by yesterday's ruling by U.S. District Judge Reed O'Connor.
Before I get to that, it's important to clarify where the list of services comes from. Again, via the Kaiser Family Foundation:
Under Section 2713 of the ACA, private health plans must provide coverage for a range of recommended preventive services and may not impose cost-sharing (such as copayments, deductibles, or co-insurance) on patients receiving these services.1 These requirements apply to all private plans—fully insured and self-insured plans in the individual, small group, and large group markets, except those that maintain “grandfathered” status. In 2019, 13% of workers covered in employer sponsored plans were still in grandfathered plans. The requirements also apply to the Medicaid expansion eligibility pathway.
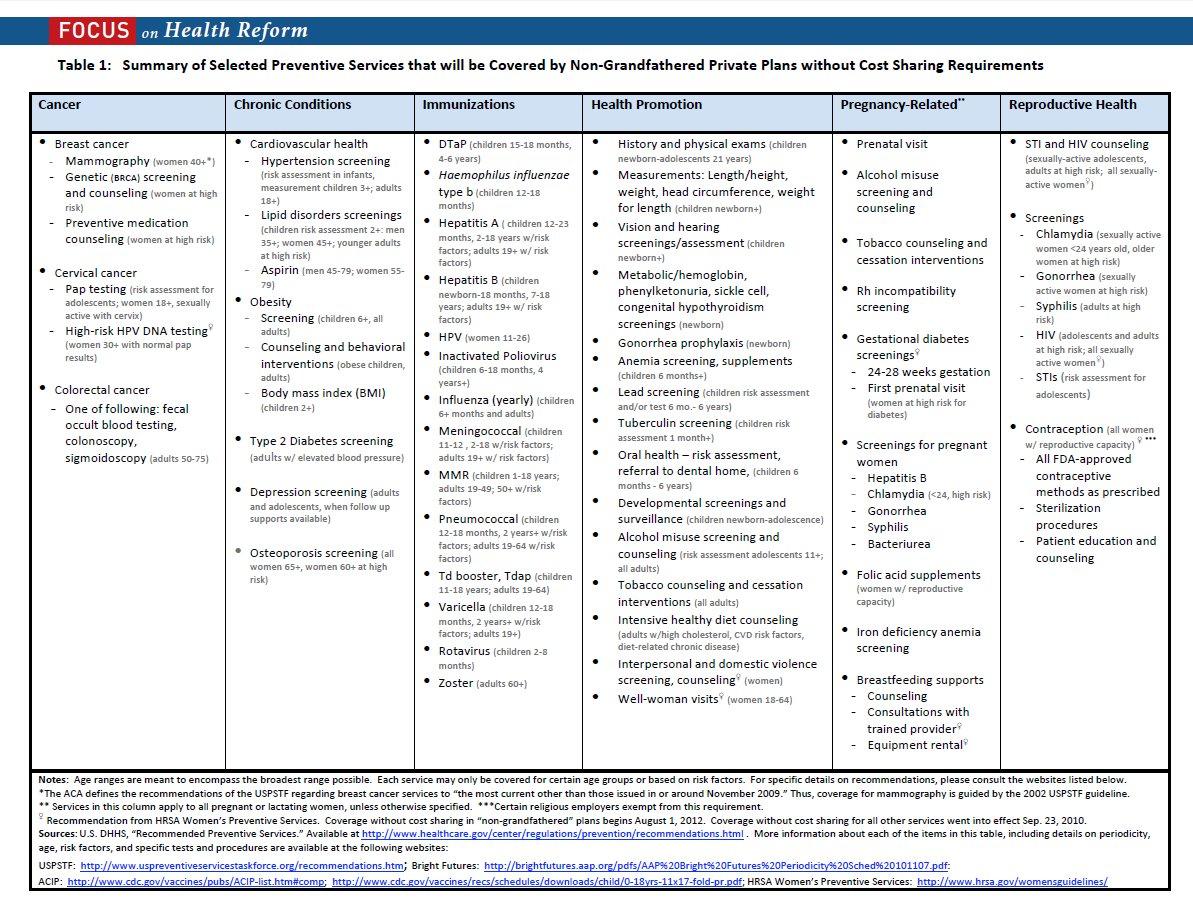
The required preventive services come from recommendations issued by four expert medical and scientific bodies—the U.S. Preventive Services Task Force (USPSTF), the Advisory Committee on Immunization Practices (ACIP), the Health Resources and Services Administration’s (HRSA’s) Bright Futures Project, and the HRSA-sponsored Women’s Preventive Services Initiative (WPSI). Individual and small group plans in the health insurance marketplaces are also required to cover an essential health benefit (EHB) package—that includes the full range of preventive requirements described in this fact sheet.
As I understand it, O'Connor's ruling strikes down coverage of HIV pre-exposure prophylaxis (aka HIV PrEP) medication as well as all services recommended by one of the above bodies (the USPSTF) made after March 2010 (when the ACA was signed into law). Apparently USPSTF recommendations made prior to March 2010 still have to be covered (I'm not sure why that distinction is included, but it reduces the scope of the ruling so that's a good thing, relatively speaking.)
With that in mind, here's Cox's explainer:
About 100 million people (6 in 10 people with private insurance) access ACA preventive services in a typical year.
— Cynthia Cox (@cynthiaccox) March 30, 2023
2. ACA preventive services recommended by the USPSTF before the ACA passed in 2010 will still be covered with $0 out-of-pocket costs. For example: breast, colon, and cervical cancer screening would still be covered without cost.
(continued...)
3. More recent USPSTF recommendations (made after March 2010) could now be subject to out-of-pocket costs. Examples include: Lung and skin cancer screenings, statins, and medications to reduce breast cancer risk (e.g. tamoxifen) (continued...)
4. When we look at the most commonly used preventive services, many of them were either recommended by groups other than the USPSTF, or were recommended by USPSTF before 2010, and would therefore still be covered without out-of-pocket costs
5/ Talk about a blast from the past: This is from my very first publication at KFF, 12 years ago, summarizing which preventive services were recommended at the time (shortly after the ACA passed)
Denying no-cost coverage of HIV PrEP medication is the biggest "prize" won by the plaintiffs. As I understand it, they basically argued that since they oppose homosexuality on religious grounds, and since some homosexuals develop HIV (as do plenty of heterosexual people, of course), it therefore somehow violates their religion to require HIV to be prevented at no out of pocket cost to other people. O'Connor agreed.
Note: Louise Norris provides a clearer explanation of their "logic:"
PrEP is for HIV prevention, rather than treatment. The ruling says that the plaintiffs believe compulsory coverage of that is "making them complicit in facilitating homosexual behavior, drug use, and sexual activity outside of marriage between one man and one woman"
No, it doesn't make any sense, but here we are.
Aside from HIV PrEP, however, the rest of the list of services which O'Connor crossed off the list gets a bit trickier, as Cox notes. First, it only applies to recommendations made by USPSTF, not the other agencies. Second, it only applies to services which USPSTF have given either an "A" or "B" rating (ie, highly recommended), since those are the only ones on the current list of mandated services in the first place. Third, it only applies to USPSTF A or B services recommended after 2010.
Even then, it gets complex because many of the services which were already given A or B ratings on the list before March 2010 have been modified since then, which means that only the pre-2010 versions are considered kosher, but tweaks made since then have been scratched out.
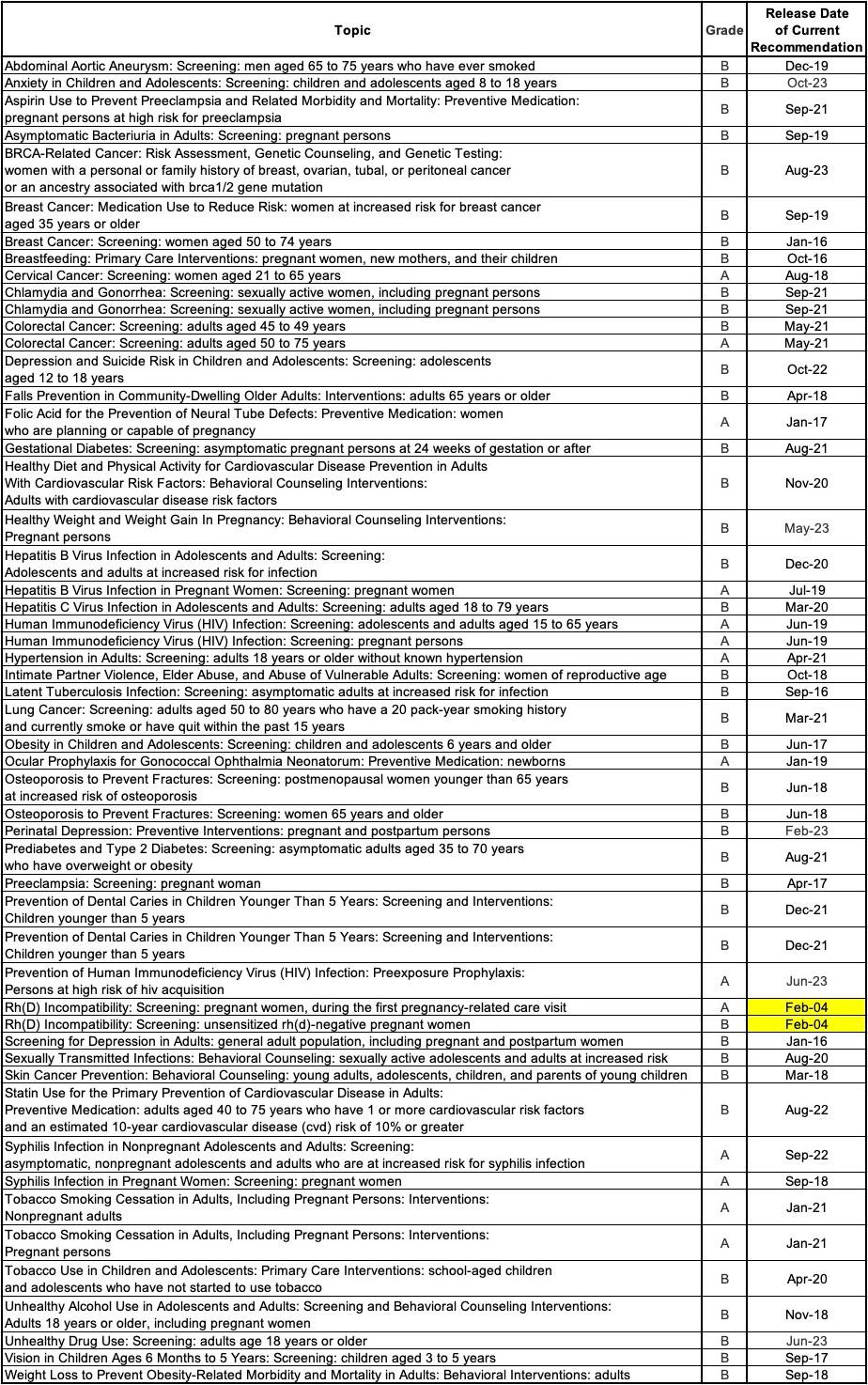
Got all that? OK, here's the full list of A & B-rated service recommendations by the U.S. Preventative Services Task Force, including the release date of the current version of their recommendations.
You have to actually click on each topic to see the details on the actual covered services--for instance, the first one (Abdominal Aortic Aneurysms) actually has recommendations for four different populations: Men 65 - 75 who have ever smoked; men 65 - 75 who haven't smoked; women of any age who haven't smoked and women 65 - 75 who have ever smoked. However, only the first group received a "B" grade, so those are the only ones who can currently have the recommended treatment covered at no charge (the recommended service itself, by the way, is a one-time screening for an abdominal aorit aneurysm via ultrasonography).
Here's a summary of the full list. Notice how there's only two (Rh(D) Incompatibility Screenings) in which either pre-date 2010 or which haven't been updated/revised since 2010:
Again, this list could shrink or grow longer depending on how the appeals process plays out over the next year or so, so stay tuned.
It's also important to reiterate several points I made in my earlier post:
- Most insurance carriers are already legally contracted to keep providing these services through the end of 2023 regardless of this ruling. The question is what happens when January 2024 rolls around. There could be a stay or injunction on O'Connor's ruling...and some carriers might decide to keep covering these services at no charge regardless, at least temporarily through the appeals process.
- There are currently 14 states (+DC) which mandate the same preventative service coverage without cost sharing to individual market enrollees as the ACA itself: California, Colorado, Connecticut, Delaware, District of Columbia, Maine, Maryland, Minnesota, New Mexico, New Jersey, New York, Oregon, Virginia, Vermont and Washington State.
- OWEVER, as Adrianna McIntyre notes, state-level protections of this nature don't (and in fact, can't legally) apply to self-insured employer plans, and as Michael Capaldo added, some may not apply to fully-insured group plans either. Capaldo says that New York's protections do apply to fully insured group plans but doesn't know the status of this in the other states.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.