Guest Post: Throwing another possible approach to healthcare policy reform into the mix
Arthur Childs, DO, FACOI is an internist specializing in critical care medicine in Cape May Court House*, New Jersey. About a year ago, as part of a project for the Jefferson School of Population Health, he put together his own Strategic Roadmap for Healthcare Delivery in the United States as a potential alternative to the various universal coverage proposals being tossed around on the left side of the aisle these days. He asked me to read it over and wanted my feedback.
I've done so, and while I'm still a strong proponent of going the Medicare for America route, he makes a lot of useful points and provides much food for thought. It's also very well-researched and cited, and I felt it deserved a wider audience. And so, with the permission of both him and the Jefferson School of Population Health, I'm presenting his full paper with a few of my own thoughts interspersed.
*(yes, that's the actual name of the municipality)
Introduction
The history of healthcare delivery has evolved from a simple doctor-patient relationship to a $3 trillion / year network of complexity and fragmentation that threatens to consume our national GDP. This evolution has led to the degradation of our physician/provider workforce and threatens the social quality and equality of care necessary for a healthy populace (Childs, 2018).
In order to provide a future direction for success, we must be cognizant of the external forces that threaten forward thinking; realizing that the politics involved may remain polarizing for the very people we aim to support, and recommended changes may be too incremental for some, while too drastic for others. Thus, change must include strategies that simplify rather than add complexity to the system and must be based on value, quality and evidence-based facts.
The following outline introduces four basic objectives that aim to improve the care, value and equity of our system, reduce costs, and improve patient and provider satisfaction.
- Private Insurance reform
- Primary and preventative care access
- Profit margin redistribution to research development and patient care
- Promotion of evidence-based medicine
Considering the divisive politic the United States faces, any plan must include incentives that are amenable to both sides of the political spectrum, are easy to implement and reduce rather than add complexity to the system. Keeping this in mind the following is a summary of objectives and a roadmap for implementation and acceptance.
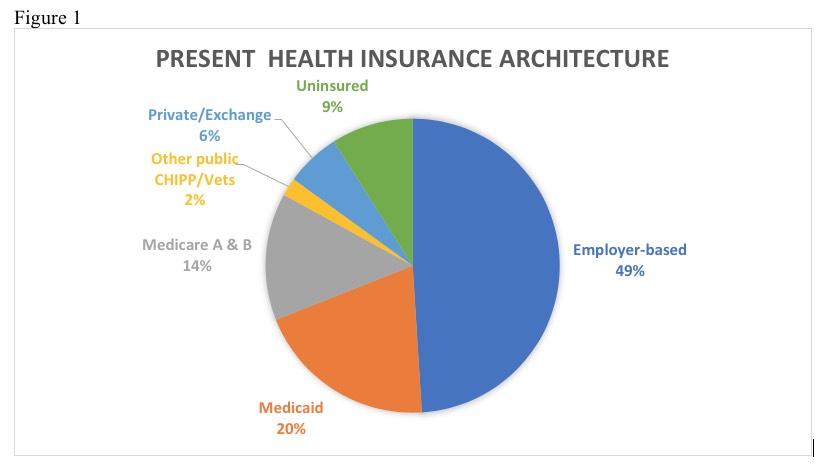
Insurance Reform
The purpose of insurance is the ability to mitigate one’s exposure to risk and protect assets against catastrophic loss. Historically, the healthcare delivery system of the US has used insurance to pay for disease episodes but failed to include preventative measures and efforts to promote health (Shi & Singh, 2019). It was not until recently with the passage of the Patient Protection and Affordable Care Act (PPACA) that insurance carriers became responsible for essential health benefits to cover preventative care as well as pre-existing conditions. While the pool of uninsured individuals was considerably reduced with the creation of health insurance exchanges and Medicaid expansion, 28 million individuals still remain uninsured ("KeyFacts," 2017). Despite the PPACA’s 80/20 rule that reigned in profits by reinvestment in health care, private insurance companies still profit tremendously by being the insurers of the healthiest and least at-risk population. While covering 56% of the insured in this country 36% are left to the Public Trust mostly through Medicare and Medicaid coverage (Shi & Singh, 2019). Furthermore, 49% of insurance is employer based, which amounts to a significant economic burden placed on employers and the public to keep up with rising premiums. Many have argued that this has been a major determinant preventing wage growth in our workforce (Tracer, 2017).
I absolutely agree with this last point, and it's why, ironically, even as a strong supporter of the ACA as a whole, and even as someone who supports having an the individual mandate, I've actually called for the elimination of the employer mandate instead...but only after major improvements are made to the ACA subsidy structure first. The combination of these factors would lead to a gradual shift away from employer coverage and towards the individual market...making it in turn easier to transition to whatever new system comes to replace the current one.
While the PPACA was successful in decreasing the total uninsured population, the full benefits of the plan have not been realized. This has been attributed to the removal of the mandate by the current administration and decreased acceptance and support by many states of Medicaid expansion and health insurance exchanges. The Republican party ideologically finds government control anathema to any health care changes and encourages choice of coverage with lower premium catastrophic plans. They have also recently reintroduced short-term insurance plans that may be cheaper yet do not provide the comprehensive coverage necessary to maintain a healthy population (Luhby, 2018). On the other side of the isle the PPACA introduced a concept into the public psyche that Health Care is a Right, a mantra echoed by the World Health Organization’s constitution envisaging “The highest attainable standard of health as a fundamental right of every human being” ("WHO human rights," 2017).
As I've noted many times before, whatever other successes or failures the ACA has had to date, the single most important accomplishment is completely changing the zeitgeist of the American public. We've gone from shrugging off those discriminated against for having pre-existing conditions as being an unpleasant fact of life to being unacceptable...which in turn leads to the question, "OK, if that's the way you feel, what should we do about it?"
That's what the next major healthcare debate (which this post is part of) is all about: What should we do about it?
The mental and physical health of our population is a national security priority ("Natl Health Security," 2018) and as such should be paid for utilizing public funding. Compromise is necessary in designing plans that aim to be successful in the eyes of the entire political spectrum. Additionally, it must maintain an easily workable structure based on present day system architecture. The following proposal uses as its core the idea that meaningful insurance reform must include the decoupling of catastrophic care coverage from primary preventative and chronic disease management.
This is the core of Dr. Childs' proposal. Again, I don't necessarily agree, but it's worth hearing him out.
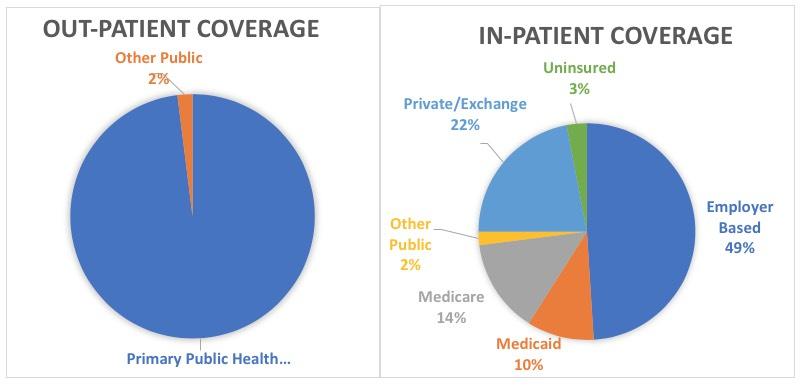
Using the present Medicare Part B architecture, outpatient preventive and chronic disease management should be separated out from private insurance. With a combination of payroll insurance and general tax revenues, funding would be used to cover outpatient care and provide primary care access for all citizens. As a result, employer-based funding of high priced private insurance plans would shift to much cheaper catastrophic plans that cover in-patient services similar to present Medicare A coverage. Individuals and families will pay into this public system, let us call it Medicare PPH (for Primary Public Health), utilizing a scaled tax system that will exercise needs-based income subsidies for patients up to 400% the poverty level. Although the Supreme court upheld the constitutionality of the healthcare mandate as a tax (Liptak, 2012) it will be more palatable, as well as guarantee universal coverage, to have funding incorporated into general tax revenues with much of the profits now realized by private insurers being used to reduce the overall tax burden.
This is an interesting point. I've often pointed out that while "Medicare for All" advocates often insist that MFA "wouldn't require an individual mandate!", the truth is that single payer healthcare systems have their own "individual mandate"...it's just called "pay your taxes". People tend to be less likely to protest at an automatic tax deduction (think FICA or existing Medicare or SSI taxes) than they do being hit with it as a separate line item all at once when they file annually.
The average individual health insurance yearly premium in 2017 was $4716 and deductibles on average increased this price tag by $1021. Consequently, individuals are paying over $5k a year and families over $20k a year for a decent plan, a price tag that is untenable and continues to rise ("Obamacare rate review," n.d.). Employers who represent 49% of our health care insurance funding thus stand to benefit a great deal by changing over to catastrophic type plans, which on average only cost $1999/year per individual ("cost of health insurance," 2017). In addition, an estimated $250 billion per year of revenue is lost through tax credits for employer-based coverage ("CBO," 2016). A significant reduction in employer-based insurance costs would therefore have a proportional effect on the revenue lost by this tax credit (McClanahan, 2017). The federal government covers over 62% of Medicaid costs which is commensurate to over $300 billion spent per year. With this proposed system, the $140 billion plus currently being paid towards managed care plans will significantly be reduced since these plans no longer will need to cover primary care (McClanahan, 2017). By leaving the same private and health exchange insurance architecture in place and returning insurance to its original missionmitigating catastrophic riskwe, as a country can begin to focus on primary risk prevention, and health promotion.
I can't stress the $250 billion/yr in employer-based health insurance tax deductions enough. The combination of this tax deduction plus employers covering the bulk of employee premiums serves the same function as the ACA's APTC & CSR assistance...the difference being that the employer "subsidies" don't cut off at 400% of the Federal Poverty Line.
Medicare PPH, will increase the pool of healthy low risk individuals enrolled in our public health delivery system. These individuals, in turn, will help maintain manageable costs for the system in place and replenish profits for better value-based initiatives and public preventative care. In-patient care costs will now be covered by employer / exchange and private based catastrophic plans, and the remaining percent of the population will stay on present Medicare A, Medicaid and Veterans reimbursement strategies. Since Medicaid enrollees will now have outpatient coverage on Medicare PPH, outpatient reimbursement will be increased to levels more representative of the care provided, improving access to care in a more equitable fashion. In addition, by enrolling all individuals, the 28 million people presently without access to primary care other than through emergency services will now have access to care. For ease of transformation, at first, the coverage strategies should be based on similar rules and regulations as is seen with current standards for Medicare A and B participants.
It sounds like this would basically amount to a universal single payer system...but only for general healthcare treatments. Annual physicals, blood screenings, mammograms, vaccinations, physical therapy and the like would be paid for entirely via taxes...but catastrophic care (hospitalization, chemotherapy, dialysis, etc...the expensive stuff) would still be handled via private insurance.
This is actually the exact opposite of some proposals I've heard (usually from Republicans), which push for universal catastrophic care (also involving private insurance carriers, of course), but want to leave individuals fully footing the bill for their preventative and chronic management expenses.
In order for the Primary Public Health Plan to truly embody the WHO’s objective of “the highest attainable standard of health,” coverage must evolve over time, fostering health and access as a means of reducing costs and increasing value in the eye of the public as well as private systems. Therefore, we must discuss our next objective, primary and preventative care access.
Primary and Preventative Care Access
Primary care is defined in the United States as “the provision of, integrated, accessible health care services by clinicians who are accountable for addressing a large majority of healthcare needs, developing a sustained partnership with patients, and practicing in the context of family and community.” (Starfield, Shi, & Macinko, 2005). It is the specialty that creates the greatest health value for the nation. Numerous studies have presented evidence that primary care is strongly associated with the prevention of illness and death as well as the promotion of a more equitable healthcare distribution (Starfield et al., 2005).
Unfortunately, we face a looming shortage of primary care physicians. Estimates indicate that the US will be short 90,000 primary care doctors by 2025 (Association of American Medical Colleges, 2015). Inadequate access to primary prevention and care for chronic conditions remains a major impediment to individual and population health in our country (Childs, 2018). This reduced primary care workforce can be attributed to many factors including mounting pressure for clinicians to choose more lucrative specialties in the face of rising student debt as well as length of training. Many cite the significant income gap between primary care and specialty reimbursement in the context of increased workload and high burnout as another contributing factor (Bodenheimer, Berenson, & Rudolf, 2007).
I've often pointed out that one of the reasons (though not by any means the only one) that "every other developed nation on earth!" manages to achieve universal coverage for so much less than the U.S. is because in some countries medical school costs far less, either due to much of it is being subsidized by the government or other basic economic differences unique to that country. Meanwhile, in the United States, the average medical student graduates and hits the ground running a good $170,000 in debt. That's a lot of pressure for a new doctor to go into a high-pay specialty even if they really didn't become one "for the money".
It also doesn't help that many feel that Medicare tends to underpay primary care physicians and pediatricians compared to specialists.
Discussions regarding a strategic roadmap for healthcare must include a comprehensive plan for improving access to primary care. Inclusion of dental services has also shown to improve overall health and should be included as well. Federally funded community health centers already serve as a model for comprehensive health. Areas that are served by community health centers are proven to be healthier than populations with comparable levels of social deprivation that receive care in the form of clinics and other kinds of physicians’ offices (Starfield et al., 2005). Our goal for comprehensive healthcare can be achieved by utilizing well accepted concepts of the Patient Centered Medical Home (PCMH) (Patient-Centered Primary Care Collaborative ,2017). By integrating access for behavioral and mental health, addiction care, patient navigators and chronic care management we can truly come closer to our goal of comprehensive health care.
As an aside, I have never understood why dental and vision care has always been kept separate from "major medical" insurance policies. There are some policies which include them, but they're pretty rare and it's still treated as some sort of bonus or extra. Eyes and teeth are part of our body, aren't they? No one buys a standalone "Nose Policy" do they? Weird.
Community health centers presently serve 25 million patients at a cost of $516 per patient per year yet they have the structural capacity to serve 50 million (McClanahan, 2017). Other countries spend much less than the US on healthcare and possess better outcomes, which is partially a result of these countries’ intentional expansion of primary care access for all of their citizens. Spain, for example, introduced legislation in the 80’s to provide community health center access within a 15-minute radius of every person. The establishment of new centers that model primary care excellence in addition to increased funding and services can provide improved access for better health and better productivity of our workforce (Starfield et al., 2005).
In addition to increasing primary care infrastructure, our goals require us to entice more providers to pursue primary care. Alternative Value Based payment programs like those successfully employed by the CMS Primary Care Plus (CPC+) model provide greater financial support for staffing and physician salaries. With a CPC+ payment model, FFS payments are reduced in favor of global evaluation and management services payments thus making practices “incentive neutral” giving providers better flexibility to deliver unrushed care in a manner that meets the needs of the patient and provider ("CPC-plus," 2018). Under the new Medicare PPH plan, all payments would be uniform, streamlining the unnecessary difficulties associated with billing and precertification.
Performance based incentive payments (PBIP) can be used to reward and maintain quality and benchmark care needs. This will clearly improve patient as well as provider satisfaction and entice more physicians into primary care (Sessums, 2016). Current trends indicate that more primary care physicians are being forced into employment arrangements with large healthcare systems (Muchmore, 2018). Many private corporations and private equity firms continue to enter the field of primary care upon the realization that employee health is paramount to retention, productivity and profits (Kutscher, 2015). As long as we maintain value as the incentive for reimbursement, competition will drive the infrastructure needed to meet the needs of the larger patient pool. Since payments will be controlled solely by the PPH plan, all private or public-private PCMH enterprises can be required to conform to minimum standards of care, access, and staffing needed to provide comprehensive preventative and chronic disease management.
We can also incorporate a PGY1 PCMH internship with payment and residency incentives inspired by prior AOA requirements for rotating internships, to involve and thus educate medical graduates in systems based, value-based, primary preventative care. Eventually, these medical homes will include general sub-specialties providing for an optimal learning experience for all.
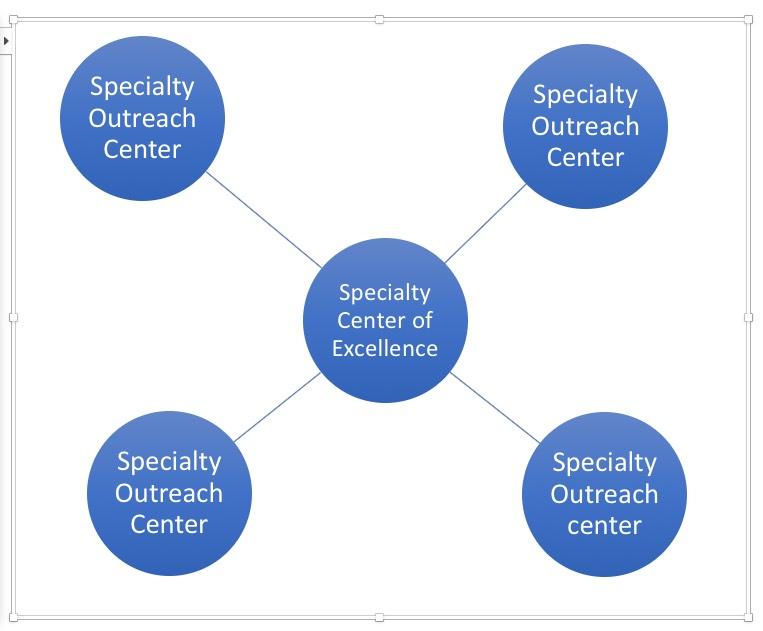
Estimates show that it costs about $1000/person per year to provide the comprehensive primary care and chronic disease management in community health centers that we envision (McClanahan, 2017). PCMH transformation programs across the country have already shown savings of $26.37 lower per member per month in adult medical costs. Considering that the US spends over $10,000 per person/year on health care, the idea of providing comprehensive access is well within reach, especially since overall health costs diminish with increased value-based primary care access. These model strategies are associated with reduced hospital and emergency department utilization, reduced costs, higher preventative care measures, and screening rates for patients regardless of socioeconomic status (Patient-Centered Primary Care Collaborative,2017). The inclusion of mental health, addiction treatment and care will allow us to realistically address the ever-growing opioid epidemic we now face. As technology advances and more surgical procedures shift to the outpatient setting we would expect to see a concomitant increase in PPH costs. Similarly, as life expectancy increases there should be greater use of outpatient services such as with dialysis and chemotherapy. However, taking into account the significant expected increase in population health, preventative screenings and care we expect with our program such costs will actually decline. Utilizing Value Based incentives we envision hub and spoke surgical and medical subspecialty systems to emerge. There will be Value Based Centers of Excellence at the Hub and outreach local specialists competing for value, performance and quality rather than demographics.
Again, as an aside: The life expectancy issue is one which we, as a society, have been ill-equipped to deal with in a lot of areas. Long-Term Services & Support is likely to be the fastest-growing sector of healthcare expenses soon if it isn't already. This is why I'm glad to see that the Medicare for America bill includes LTSS as part of the core services covered.
As quality, population and preventative health improves we will see a positive shift in life expectancy. How to deal with a growing elderly population is already a daunting task. Using our PPH/PCMH, Hub and Spoke specialty model we can apply similar strategies to the creation of geriatric centers of excellence situated throughout assisted living, short and long-term nursing facilities across the country. By using Medicare PPH in conjunction with an improved primary care infrastructure we can finally be a country that achieves equity in healthcare delivery that not only treats disease but promotes and provides good health
Profit Margin Redistribution to Research Development and Patient Care
Prescription drug expenditures presently account for more than 12% of total personal healthcare costs in the US. Despite record setting profit margins in the Pharmaceutical Industry, the retail price of expensive brand name drugs and generic drugs have skyrocketed. Sales revenues have grown from $534 billion in 2006 to $775 billion in 2015 aggravating the economic burden on our healthcare system (United States Government Accountability Office [GAO], 2017). With annual profit margins anywhere between 15- 40% compared to the top 500 non-drug companies whose margins are between 4-9% we can see why Big Pharma reform is crucial to the future direction of US healthcare reform (Throng, 2015).
Many politicians on both sides of the political spectrum have called for price controls as a means of reducing rising costs. Big Pharma has pushed back claiming that price controls would reduce R&D and thus make it impossible to bring new drugs to market as brand drugs come off patent. However, company reported R&D spending increased only slightly from $82 billion to $89 Billion between 2008 through 2014, with only a modest portion of this increase allocated to research and development of new drugs. In fact, we have seen a sharp rate of decline in R&D over the past ten years which one health economist has coined “Eroom’s Law “as the reverse of Moore’s Law to describe the exponential decrease seen in R&D (Throng, 2015).
In other words, the "it'll hurt R&D!" arguement is mostly bunk.
The inability for Medicare to negotiate retail drug prices, enables price instability. Price gouging by companies that have a monopoly on certain drugs are only recently catching the public’s ire and stimulating prosecutions and large penalties (Staples, 2017). According to the literature, Comparative Effectiveness Research(CER) programs improve quality and reduce costs by comparing existing health care interventions and treatments to determine which therapies work best and which pose the greatest harms. Ongoing research into existing therapies is thought to be a major route for improved care. For example, research can allow for the adoption of already marketed interventions for other applications reducing the overall cost of drug development while increasing the therapeutic options available to the market. (Institute of Medicine, 2009).
While these seem like simple fixes, the Pharmaceutical Industry is a very complex world where multiple factors are at play. While CER’s are a great idea, studies show that as CERs increase R&D declines challenging novel health care innovation (Vernon, Golec, & Stevens, 2012). Over the past 10 years increased mergers and acquisitions have increased profits and appeased stock holders by raising drug prices, consolidating manufacturing and pursuing products with inherently lower risk. These mergers and acquisitions have also led to greater market dominance and less competition thus leading to the doubling and even tripling of drug prices. Many companies by acquiring or paying generic competitors, delay releasing less expensive alternatives thus maintaining the high price of brand products (DeAngelis, 2016).
I should note that the House Energy & Commerce Committee just this week forwarded six different prescription drug regulation-related bills to the full House floor...several of which had true bipartisan support, including making it illegal for brand-name drug companies to basically bribe generic drugmakers to keep generics off the market, and to require it to be easier for generic makers to acquire proper samples to develop the generics.
Alternatively, by acquiring promising new or developed research and product lines, a merger or acquisition may help companies mitigate R&D investment (GAO, 2017)). Pharmaceutical companies are not alone and there are programs to incentivize drug development through patent and market exclusivity as well as grants from agencies such as the NIH. Tax incentives have also been created such as the Orphan Drug Credit, Research Credit and deductions for Qualified Research Expenses Programs (GAO, 2017). Despite these efforts, profits continue to climb out of proportion to R&D investment and the public is faced with pharmaceutical companies paying more money to market drugs than develop them (DeAngelis, 2016).
We must find a way to regulate the skyrocketing profits of Big Pharma and redirect them to patient care research and development. 20-40% profit margins for an industry that is reducing R&D and overcharging a captivated public must be dealt with in a way that maintains profits, reduces costs and promotes new innovative therapies based on the public’s needs. Thus, we propose the following:
- As was done with the 80/20 medical loss ratio rule of the PPACA ("Obamacare rate review," n.d.), a similar strategy should be used for reinvestment of profits back into health initiatives. These funds should be dedicated to R&D including Orphan drug research, CER and continued manufacturing of life line drugs that are needed for ongoing care but presently are not, due to low profitability. Legislation should be crafted that incentivizes transparency and a pay for value rather than pay for monopolization of high cost drugs.
Aside: This is exactly what I proposed back in April 2017:
14. INSTITUTE AN 80/20 MLR POLICY FOR PHARMACEUTICALS.
...Under the ACA, insurance companies are legally required to spend at least 80% (85% in the case of large group plans) of the premiums paid on actual healthcare services rendered--they can only earn a gross profit of up to 20% (15%) for overhead. This is meant to cut down on expensive junkets to Tahiti, marble staircases in the corporate headquarters and so forth.
Unfortunately, the ACA has no similar provision for drug manufacturers. There's not a whole lot which can be done about a pharmaceutical company raising prices through the roof whether they "need" to or not (yes, it's extremely expensive to develop a new medication, but sooner or later that cost is amortized and the rest is mostly gravy).
Getting back to Childs...
- Marketing of pharmaceuticals to the public should be banned. While there is a place for marketing when dealing with population health initiatives and marketing of novel techniques, specific brand marketing does nothing but supersede the clinician’s clinical judgement and waste valuable resources.
I remember a time when pharmaceutical companies weren't allowed to identify a specific prescription drug by name--they'd run TV commercials saying something like "If you have symptoms X, Y and Z, there may be a solution! Ask your doctor!"...and then close with the company logo, in the hopes that the patient would describe the commercial and the company name to their doctor, who would presumably know what drug they were referring to. We've been long past even that layer for awhile now.
- We must invest in increased NIH funding and public-private partnerships to promote new innovative lines of research and novel therapies that address the needs of the population at large.
Using our Medicare-PPH platform, as essentially the sole negotiator for drug therapy, will allow for better negotiated prices from manufacturers and PBM’s. Redistribution of profits will allow for better reinvestment and if done correctly can reduce overall costs while still promoting value, offering a way forward with innovation that is not industry driven but patient and population needs driven.
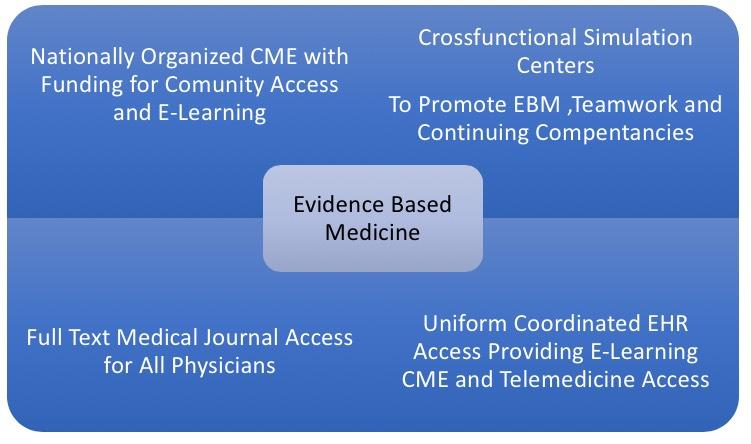
Promotion of Evidence Based Medicine
Evidence based medicine (EBM) is defined as the “conscientious, explicit, judicious and reasonable use of modern, best evidence in making decisions about the care of individual patients’ (Straus, Glasziou, & Richardson, 2010). EBM necessitates the integration of the clinician’s experience and expertise along with a recognition of patient values and the most current available scientific clinical evidence (Straus et al., 2010). Without updated dissemination of evidence-based guidelines clinicians may not be following updated algorithms for preventative and clinical services thus leading to potential overuse of resources and outdated and potentially harmful therapies. The integration of these factors is imperative in making choices regarding patient care. Unfortunately, the pace of scientific discovery is so great that many clinicians have trouble keeping up with the data and science. Physicians have less and less time available to devote to reading medical literature and when they do many only have time or access to read only the abstract of a paper which can in many cases be misleading. That coupled with the lack of training in critical skills needed to critique medical literature and we can see why the time from validation to implementation of a new clinical practice is, shockingly, 17 years (Stoneking, Denninghoff, Deluca, Keim, & Munger, 2011).
CME programs are inherently expensive to run especially at local community hospitals and very often get outsourced when competing for scarce funds (Mazmanian, 2009). While many metropolitan health facilities have the benefit of being associated with higher education faculties, medical school educators, cme programs and simulation centers, most community and rural medical staff do not. In larger teaching institutions with access to simulation centers, cross-functional simulation has been shown to improve clinical team performance when added to an existing didactic teamwork curriculum (Shapiro, Morey, & Small, 2004). Additionally, simulation has been used to benchmark clinical skills of individuals and groups over time, allowing for the identification of interventions that improve clinical effectiveness (Mah, Bingham, & Kirton, 2009). The cost for full text access to relevant clinical medical literature can be expensive to individual practitioners that do not have University privileges.
This is something I haven't thought about in decades, but I do remember my father (who was a family physician himself in the 1960's - 80's) complaining about the massive backlog of medical journals, papers, seminars and so on that he was constantly falling behind on. These days it's easier in some ways thanks to the internet, streaming video and so forth...but that doesn't create any more time for a busy doctor to keep up.
In order to achieve high-value healthcare and pursue a broad system of linked goals that Berwick has coined the Triple Aim (Berwick & Whittington, 2008) our strategic roadmap must include better access to evidence-based guidelines. Our proposal includes the following measures:
- Open, full text medical journal access for all licensed physicians and providers. In order to identify and close the gaps between current clinical practice and optimal practice, clinicians must have access to up to date research and best practices. Reading just the abstract does not take the place of systematic and effective scientific review. In our present world where Journalistic stewardship can be suspect, and conflicts of interest abound it is imperative that clinicians be able to have access to critically read scientific texts in their entirety for better diagnosis prognosis and therapy (Subramanyam, 2013). Utilizing present licensing fees, funds should be directed to allow ongoing / full online access to medical literature.
- Funding should be set aside for the expansion of cross functional simulation centers that may be used to promote team-based learning to keep clinicians up to date with novel as well as every day therapies and procedures. These centers can be fixed as well as transportable allowing for better access and continued education in urban as well as rural centers. Simulation has been shown to be effective in improving self-reported increased knowledge and improved clinical performance (Weller 2012). It has been used for a wide variety of clinical education initiatives from simple procedures to complex care issues as is seen with sepsis and septic shock, therapeutic hypothermia and cardiac arrest (personal experience). Simulation may also be used to help maintain competencies at the local level and reinforce evidence-based guidelines. In order to reduce costs and improve access, regional networks could be used to coordinate the development of learning programs share infrastructure costs and coordinate standards for simulation training programs and staff accreditation (Weller & Nestel, 2012).
- CME programs must be organized at the national level. Using a web-based infrastructure learning process, CME should be offered, funded and readily available at the community level. These programs should be based on evidence-based guidelines with curriculum directed toward specialty integration and population needs. These programs can be tied to value-based reimbursement and incentivized with bonuses for continuing learning. Once our Medicare PPH system is up and running the EHR platform should be uniform across the country incorporating E-learning, CME, telemedicine and population and genomic health technology that is easily accessible and coordinated throughout the country.
Conclusions
The complexity of the US healthcare delivery system has led us to the costliest system in the world. Despite healthcare spending at 17.9% GDP and estimates indicating continued growth by 2020 to 20% GDP, the United States continues to be outperformed by all other developed countries in all major determinants of health (Shi & Singh, 2019). “Fixing” the US health care delivery system therefore has become one of the most important goals of the 21st Century. How to do so has become the most important question of our times and has topped the national debate for the past 30 years. History has shown, however, that there is no easy fix to this problem. The country remains divided on the extent that Government should be involved with opinions ranging from allowing the free market to rule, to full government takeover of health services, the so called Universal Healthcare. The US delivery system does not work on true free market principles since private and public interests act as intermediaries, making decisions for patients rather than market forces (Shi & Singh, 2019). Full government takeover, however, would be political suicide in a divided electorate thus leaving any rational approach to change somewhere in the middle.
The Institute of Healthcare Improvement has adopted Don Berwick’s Triple AIM as the framework necessary when considering any change to the system. It has been advised that the three dimensions of the Triple Aim: 1. Improving the patient experience of care (including quality and satisfaction), 2. Improving health of populations and 3. Reducing per capita cost of health care, must be addressed simultaneously for any program to succeed ("IHI," 2018).
Utilizing a framework that encompasses these goals we have proposed a path forward that is achievable within 5-10 years. We have proposed insurance reform that decouples catastrophic care coverage from primary preventative and chronic disease management, thus reducing total insurance costs and restoring equity in public health. By promoting public /private partnerships in creating a vast network of value based PPH community health centers and using a PCMH/CPC-+ model for reimbursement puts us on a path to truly achieve universal access of care. Our proposal for Big Pharma maintains profitability while steering the industry towards more reasonable prices and increased research and development. By redistributing profits and making sure the public’s present, as well as future therapeutic needs are met, the industry can continue to grow while ensuring further innovation for the future. Finally, by restoring educational processes back to the forefront of healthcare delivery we can hopefully improve the time it takes from validation to implementation of evidence-based medicine. By ensuring equal access to all providers, improving electronic and point of service learning and putting the word meaningful into “meaningful use” physicians on the front lines of medicine will be more educated and up to date on the most recent quality initiatives, thus being able to deliver better quality care. Through our PPH plan we can envision every individual at birth receiving a PPH EHR Card that will make their health record portable and accessible to all their providers throughout their life time. This has already been successful in many countries around the world and by using current smart card technology will simplify and speed up administrative tasks, optimize healthcare costs and promote better quality care (Sembritzki, 2014).
By utilizing existing healthcare public and private infrastructure, sharing free market as well as government sponsored economic principles and restoring equity to primary preventative and chronic care delivery we can finally envision a world where a value-based quality informed doctor-patient relationship can be restored to decisions about health and disease rather than costs and access.
Childs goes on to include various charts, graphs and footnotes citing all of his sources, of course.
As I note, I agree with a lot of his ideas. I'm not a big fan of separating out preventative/primary care from catastrophic care, but I understand his logic. The larger point is, once again, that the healthcare system is absurdly complicated and would still be so if we moved to a universal single payer (MFA)-style system, the Medicare for America framework which I'm a big fan of, or any other system. Some areas would be less complicated...but others would be more so. Everything is a trade off, so it's mostly about what we as a society value most.
Figure 1
De-coupling of Catastrophic /In-patient from Outpatient Preventative & Chronic Care Insurance:
Note: Percentages are estimates used for illustrative purposes only. Depending on timing of implementation CBO estimates may change. Uninsured population is projected to be reduced significantly as PPH plan is implemented and in-Pt coverage costs are reduced. As wages rise due to decreased employer costs and improved outpatient access, we estimate significant reductions in Medicaid recipients as more become enrolled in private /exchange plans.
Figure 2
Increasing Primary Care Access with expansion through PPH:
- Doubling Community Health Centers from 25-50 million
- Promotion of Public-Private PCMH Centers Through Value Based payments and CPC+ reimbursement strategies
- Recruitment of Primary Care Physicians with improved reimbursement, Value based care, Lifestyle/workplace incentives, Comprehensive services and PGY1-PCMH Internships.
- PCMH/PPH Incorporation of alcohol /addiction/ mental health counseling and care
- Expansion of PCMH /PPH centers with Hub and Spoke Value-based specialty centers of excellence
- Value Based Centers of Excellence with Surgical and Medical Subspecialties forming Hub and Spoke Outreach Centers providing specialty access to all PCMH’s.
Figure 3 Redistribution of large Profit Margins promoting patient driven value and innovation
BIG PHARMA
Figure 4 Promotion of Evidence Based Medicine
References
- Average cost of health insurance (2017). (2017). Retrieved March 14,2018
- Berwick, D. M., & Whittington, T. W. (2008). The Triple Aim: Care, Health and Cost. Health Affairs, 27 No3.
- Bodenheimer, T., Berenson, R., & Rudolf, P. (2007, February 20). The primary care-specialty income gap: why it matters. Annals of Internal Medicine, 146, 301-306.
- Childs. (2018, February 15). Situational assessment of the US healthcare delivery system. Jefferson School of Population Health.
- Comprehensive primary care plus. (2018). Retrieved January 29,2018
- DeAngelis, C. D. (2016, March). Big pharma profits and the public loses. The Milbank Quarterly, 94.
- Association of American Medical Colleges. (2015). The complexities of physician supply and demand: projections from 2013 to 2025.
- Human rights and health. (2017).
- IHI Triple aim initiative. (2018).
- Institute of Medicine. (2009). Comparative effectiveness research.
- Key facts about the uninsured population. (2017).
- Kutscher, B. (2015, April 18). Why private-equity firms are buying up primary-care practices. Modern Healthcare.
- Luhby, T. (2018, February 20). Trump administration unveils alternative to Obamacare. CNN.
- Mah, J., Bingham, K., & Kirton, O. (2009). Mannequin simulation identifies common surgical intensive care unit teamwork errors long after introduction of sepsis guidelines . Simulation in Healthcare, 4(4), 193-199.
- Mazmanian, P. (2009). Continuing medical education costs and benefits: lessons for competing in a changing health care economy. Journal of Continuing education in the Health Professions, 29(3), 133-134.
- McClanahan, C. (2017, March 27). Rising from the ashes- a novel bipartisan approach to health care reform. Forbes.
- Muchmore, S. (2018, March 14). Hospitals acquired 5K physician practices in 1-year period. HEALTHCAREDIVE.
- National health security stategy. (2018).
- Obamacare rate review & the 80/20 rule. (n.d.). Retrieved March 14, 2018
- Patient-Centered Primary Care Collaborative. (2017). The impact of primary care practice transformation on cost, quality, and utilization.
- Private health insurance premiums and federal policy. (2016).
- Sembritzki, J. (2014). Use and development of health cards in Europe. AHIMA.
- Sessums, L. (2016, June 28). Medicare's vision for advanced primary care. JAMA, 315,Number 24.
- Shapiro, M., Morey, J., & Small, S. (2004). Simulation based teamwork training for emergency department staff: does it improve clinical team performance when added to an existing didactic teamwork curriculum? Quality & Safety in Health Care , 13(6), 417-421.
- Shi, L., & Singh, D. (2019). Delivering healthcare in America (7th ed.).
- Staples, D. (2017, July 8th). Maryland's crackdown on drug price gouging riles up big pharma. Mintpress News.
- Starfield, B., Shi, L., & Macinko, J. (2005, September). Contribution of primary care to health systems and health. The Milbank Quarterly, 83, 457-502.
- Stoneking, L., Denninghoff, K., Deluca, L., Keim, S., & Munger, B. (2011). Sepsis bundles and compliance with clinical guidelines. Journal of Intensive Care Medicine, 26(3), 172-182.
- Straus, S., Glasziou, P., & Richardson, W. (2010). Evidence-based medicine: How to practice and teach it (4th ed.). New York: Churchill Livingstone.
- Subramanyam, R. (2013, Jan-Apr). Art of reading a journal article: Methodically and effectively. Journal of Oral and Maxillofacial Pathology, 17(1), 65-70.
- Throng, R. (2015, March 31). Root causes of the pharmaceutical R&D productivity crisis. SciTechStrategy.
- Tracer, Z. (2017, September 19). Rising health insurance costs are eating into employees’ paycheck gains. Bloomberg.
- United States Government Accountability Office. (2017). Drug industry profits, research and development spending, and merger and acquisition deals.
- Vernon, J., Golec, J., & Stevens, S. (2012, October 18th ). Comparative effectiveness regulations and pharmaceutical innovation. PharmacoEconomics, 28(10), 877-887.
- Weller, J., & Nestel, D. (2012, May 21). Simulation in clinical teaching and learning. Medical Journal of Australia , 196(9).
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.