Maine: APPROVED rate hikes: 20% if CSRs are paid, 25% if they aren't
The state of Maine's insurance regulatory agency has announced the approved 2018 individual market rate hikes for the three carriers operating in the state. Louise Norris beat me to the punch:
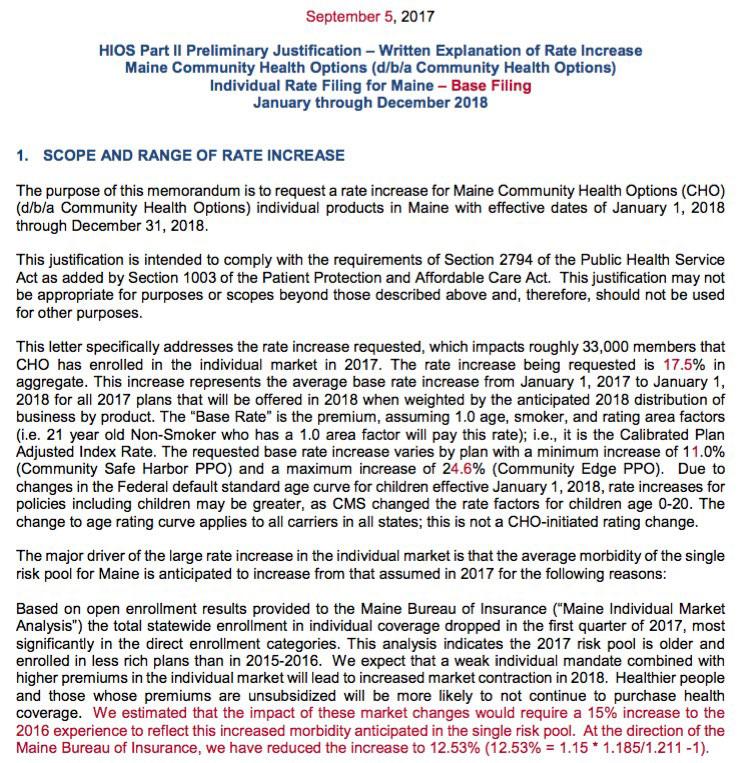
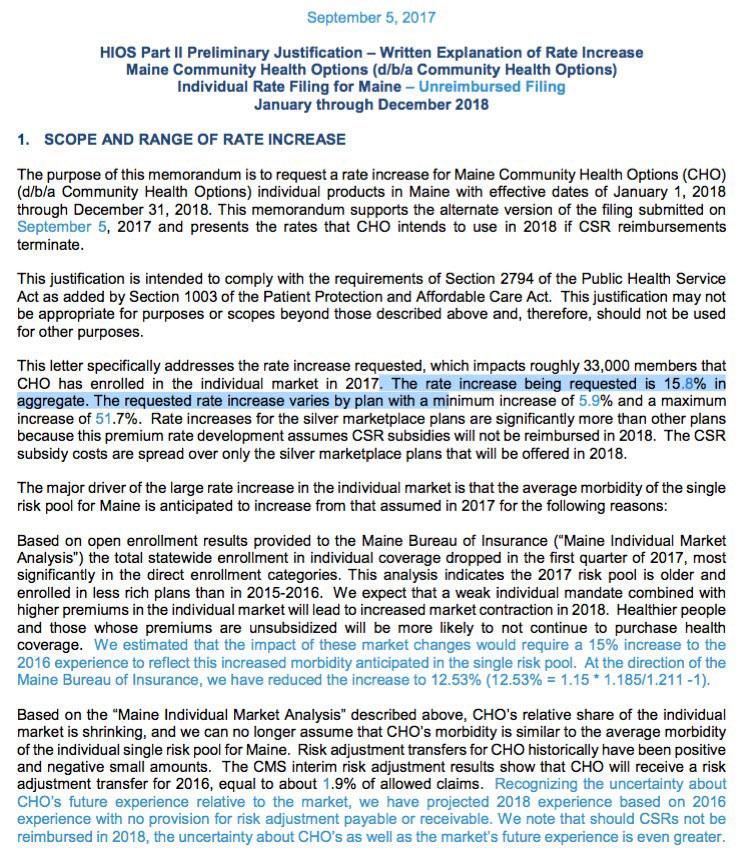
Regulators in Maine published rate proposals for the three Maine exchange insurers in June, and finalized the rates in early September. Insurers proposed two sets of rates: one that assumes cost-sharing reduction (CSR) funding will continue, and another that assumes the federal government will not fund CSRs in 2018.
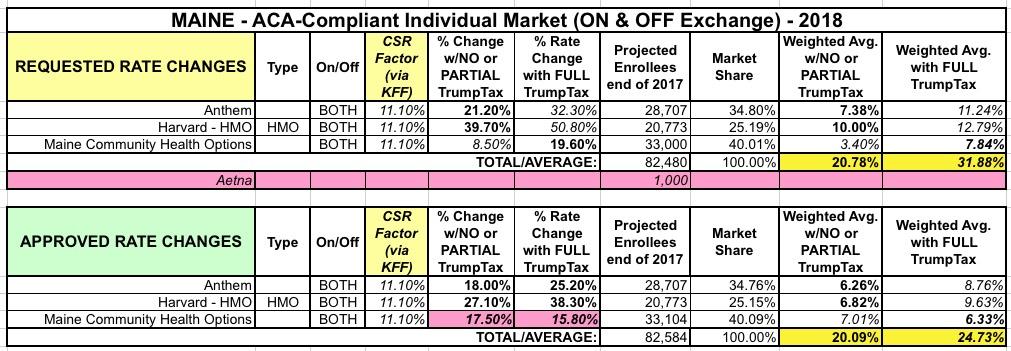
The Maine Bureau of Insurance initially rejected all three insurers’ rate proposals on August 10, and asked them to submit new rates. The revised rate filings were then approved on September 1. These average approved rate increases all assume that CSR funding will continue in 2018:
- Anthem: 18 percent (Anthem initially proposed a 21.2 percent average increase, which the Maine Bureau of Insurance deemed excessive. Anthem refiled with an 18 percent average rate increase, which was approved). The increase applies to 28,707 members.
- Community Health Options: 17.5 percent (CHO initially proposed a 19.6 percent average increase. The Maine Bureau of Insurance rejected that proposal, but noted that they would approve an average rate increase of 17.5 percent. The increase applies to about 33,104 members, and CHO expects their membership to increase to roughly 39,054 members in 2018.
- Harvard Pilgrim HMOs: 27.1 percent (Harvard Pilgrim initially proposed an average rate increase of 39.7 percent, which was rejected as excessive by the Maine Bureau of Insurance. They filed the new average rate increase of 27.1 percent, which was approved). The increase will impact about 20,773 members.
...If CSR funding is eliminated, the rate increases would need to be significantly higher for silver plans, and Anthem’s alternate rate proposal notes that they will not offer plans in the exchange if CSR funding is eliminated:
- Anthem: 25.2 percent, but Anthem plans would no longer be available on the exchange if CSR funding is eliminated. Anthem notes that they have about 28,000 individual market members now, but expect that to fall to just 5,600 if CSR funding is eliminated and Anthem plan are no longer available in the exchange. In addition to moving to an off-exchange-only model, Anthem would only market one gold off-exchange plan for new enrollees, in rating area 4. The higher average rate increase (25.2 percent versus 18 percent if CSR funding continues) reflects the overall higher morbidity Anthem expects in their membership if their plans are no longer available on-exchange and no longer actively marketing to new enrollees in most parts of the state.
- Community Health Options: 15.8 percent, but silver plan rates would increase by an average of 50 percent, while other metal levels would increase by an average of 6-19 percent.
- Harvard Pilgrim HMOs: 38.3 percent, with silver plans having an average increase of 41.7 to 45.9 percent.
I've highlighted the two noteworthy items here:
- First: Anthem's threat to take their ball and go home altogether if CSR reimbursements aren't guaranteed. Until now, I believe that Molina was the only major carrier to flat-out issue an ultimatum like this (although they followed that up by immediately firing their CEO...and then pulled out of several states anyway).
- Second: The rather oddly "reversed" rate approvals for CHO. When they requested a 19.6% rate increase, CHO made it clear that "much" of that was caused by an expectation that the individual mandate won't be enforced next year. Oddly, they didn't mention the CSR issue at all, but at the time I assumed they were also assuming no CSR payments either. However, as Norris notes, not only did the 19.6% request assume CSRs would be paid (it was cut down by 2.1 points to 17.5%), but the second rate filing--which assumes CSR reimbursements won't be made--is actually slightly lower than that (15.8%).
The actual filings are quite clear about this: The "base" filing (which assumes CSR payments) was revised to 17.5%...while the unreimbursed (NO CSR payments) version stands at 15.8%. Very weird:
In any event, when the numbers are plugged in, here's what it looks like: A small drop from 20.8% to 20.1% if CSRs are paid, and a larger drop from 31.9% to 24.7% if they aren't:
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.