New Hampshire: 92% of OE4 enrollees effectuated as of March.
According to the official CMS report for the 2017 Open Enrollment Period, 53,024 New Hampshire residents "selected a Qualified Health Plan" from the ACA exchange as of January 31st.
Of course, as I (and others on both sides of the political spectrum) have written about many, many times, not everyone who selects a QHP (either on or off the exchanges) actually pays their first premium, and therefore is never actually enrolled in an active, effectuated policy. This amounted to roughly 12-13% of all QHP selections in 2014, but has improved over the past 3 years as people got used to how the system works and technical improvements were made. I've been using a 10% non-payment rate as a general rule of thumb for some time now.
I like checking on this whenever possible. Unfortunately, CMS only released effectuated enrollee reports for HC.gov during the off-season quarterly in the past, and announced last fall that they were switching to only reporting this every six months...and that was before the November election. I haven't the slightest clue whether they'll stick to that schedule or not. That leaves it up to the 12 state-based exchanges, several of which do issue off-season enrollment reports...but even they tend to be cumulative numbers, not effectuated numbers. Massachusetts is the rare exception.
On the federal exchange, New Hampshire is the only state on the federal exchange which issues regular reports about the exact number of people enrolled in exchange-based policies every month. They even break this number out by metal level and carrier, which is very nice for tracking trends.
According to the latest report, here's how exchange-based QHP enrollment has played out for the first 3 months of 2017:
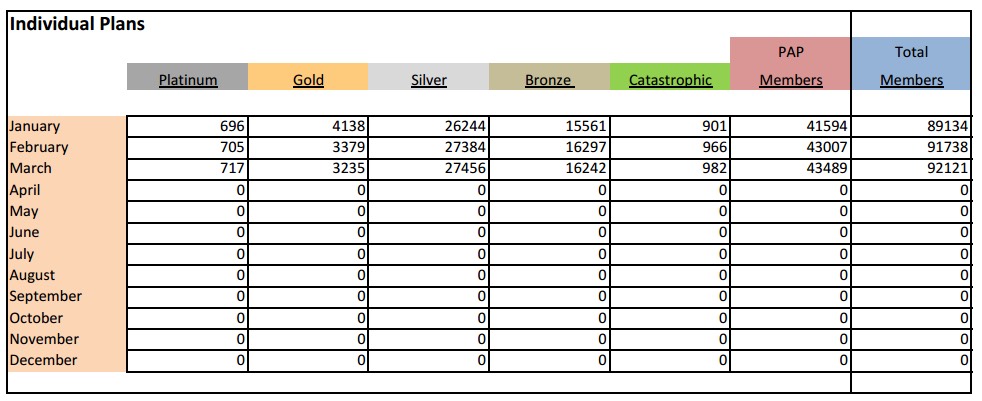
Note that "PAP" (or "Premium Assistance Program") is New Hampshire's name for their Arkansas-style "Private Medicaid Option" in which those who qualify for Medicaid expansion are, instead, enrolled in the same QHPs as other exchange enrollees...except that Medicaid funds are used to pay for virtually everything. Think of these as high-metal level QHPs with 99% APTC/CSR subsidies. They're officially categorized as being under Medicaid by CMS/ASPE, so they aren't included as QHPs in the official reports.
When you subtract the PAP numbers out, you get:
- January: 47,540 QHPs
- February: 48,731 QHPs
- March: 48,632 QHPs
That means that as of March, 91.7% of all ACA exchange QHP enrollees were still effectuated. Aside from no-pays, there's still some churn because anyone who enrolled between 1/16 - 1/31 didn't start coverage until March 1st...yet the March number is still slightly lower than February's.
New Hampshire is a small state, so there's no way to extrapolate nationally, but a 92% retention rate as of March is slightly better than I'd expect.



