UPDATE: Who will Do the Silver Switcharoo, Part Two: How many by state?
A week or so ago, David Anderson, Louise Norris, Andrew Sprung and I co-wrote an article explaining how different states were planning on handling 2018 individual market pricing given the massive uncertainty surrounding ongoing Cost Sharing Reduction (CSR) reimbursement payments.
Our timing couldn't have been more fortuitous: Less than 48 hours after we posted the piece, Donald Trump announced that, sure enough, he's finally following through on his threat to pull the plug on CSR payments, effective immediately.
It's still conceivable that the carriers will receive the CSR reimbursements for 2018 anyway, of course; in addition to the just-introduced bipartisan Alexander-Murray bill, eighteen state Attorneys General have filed for an immediate court injunction requiring the payments to continue. However, the odds of the first going through in time to reverse the already-baked-in 2018 rate hikes are almost zilch, and even if the injunction is granted, there's still a strong possibility that it'll be too late to reverse 2018 rates.
In other words, I'd say there's about a 95% chance at this point that the additional CSR cost load will be added to 2018 rates (even if the extra money is paid back to enrollees and/or the government starting in 2019). Our collective "CSR Load" spreadsheet seems to be a pretty good guide to how the states are gonna handle the situation after all.
With that in mind, where do things stand as of today? Well, there's been a lot of last-minute scrambling by several of the states and carriers which had previously crossed their fingers and hoped that CSRs would be made, and there's likely to be some more 11th hour changes to come, but as of 10am, Thursday, October 19th, 2017, here's the status of every state to the best of our collective knowledge:
- Assuming CSRs will be Paid: 2 states + DC
- District of Columbia, North Dakota & Vermont
- Broad Load across All Plans: 5 states
- Colorado, Delaware, Indiana, Oklahoma & West Virginia
- Loading to All Silver Plans: 18 states
- Alaska, Arkansas, Iowa, Kansas, Kentucky, Louisiana, Massachusetts, Michigan, Mississippi, Missouri, Nebraska, New Hampshire, New Jersey, New York, North Carolina, Oregon, South Dakota, Tennessee
- Loading to On-Exchange Silver Plans Only w/off-exchange Silver Option ("Silver Switcharoo"): 20 states
- Alabama, California, Connecticut, Florida, Hawaii, Illinois, Idaho, Maine, Maryland, Minnesota, Nevada, Ohio, Pennsylvania, Rhode Island, South Carolina Utah, Virginia, Washington, Wisconsin, Wyoming
- MIXED Load (different carriers within state using different strategies): 5 states
- Arizona, Georgia, Montana, New Mexico and Texas
UPDATE: Illinois' status changed from "Silver" to "Switcharoo". Breakout and tables have been updated to reflect this.
UPDATE: Massachusetts' status changed from "CSRs Paid" to "Silver Load". Breakout and tables have been updated to reflect this.
UPDATE: Maryland's status changed from "CSRs Paid" to "Silver Switcharoo"; West Virginia's status changed from "Silver Load" to "Broad Load". Breakout/tables updated to reflect these changes.
UPDATE: Utah's status has been corrected from Silver Load to Silver Switcharoo.
UPDATE: Virginia's status has been corrected from Mixed to Silver Switcharoo; Alabama's has been corrected from Silver Load to Switcharoo.
UPDATE: Kentucky's status has been corrected from Broad Load to Silver Load; Wisconsin and Wyoming have been corrected from Silver Load to Switcharoo..
UPDATE: Maine's status has been changed from Silver Load to Silver Switcharoo
- NOTE: The District of Columbia's strategy is unknown...but irrelevant, for two reasons: Since people earning up to 215% FPL are eligible for Medicaid in DC, only about 3% of their exchange enrollees receive CSR assistance anyway; and even among the 500 or so who do, they're only receiving around $650 in savings this year as opposed to the $2,700 - $3,200 in savings that lower-income CSR recipients receive everywhere else. So you're really talking about perhaps $400,000 in CSR cost for all of 2018 to be spread out among around 21,000 people on the individual market...or $19 per person for the whole year.
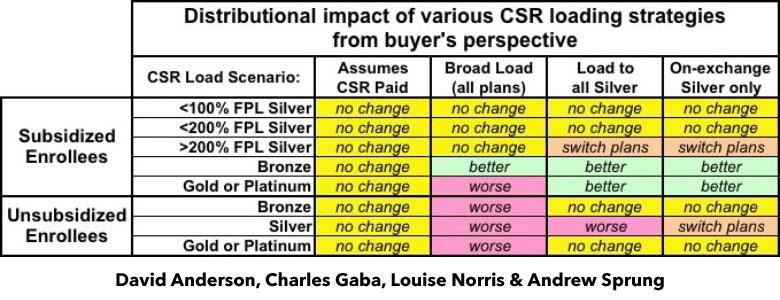
Here's a handy chart which shows (roughly) how different current enrollees should fare under these strategies depending on which state they live in:
So now the question is, just how many current individual market enrollees will be impacted by these scenarios?
I've done my best to estimate these. It's important to keep in mind that this involves quite a few estimates and assumptions, including:
- I'm assuming that our spreadsheet as it stood this morning is accurate and doesn't change further
(it will, of course)
- I'm assuming that every single person currently enrolled in an ACA-compliant individual market policy remains in an ACA-compliant plan
(not all of them will, of course; some will drop coverage entirely and pay the mandate penalty fee)
- I'm assuming that everyone eligible for subsidies in 2017 will also be in 2018, and that no one NOT currently eligible will be next year
(some will change their status both ways)
I'm going to start with the ACA exchange-based enrollees, and will then look at off-exchange enrollees later.
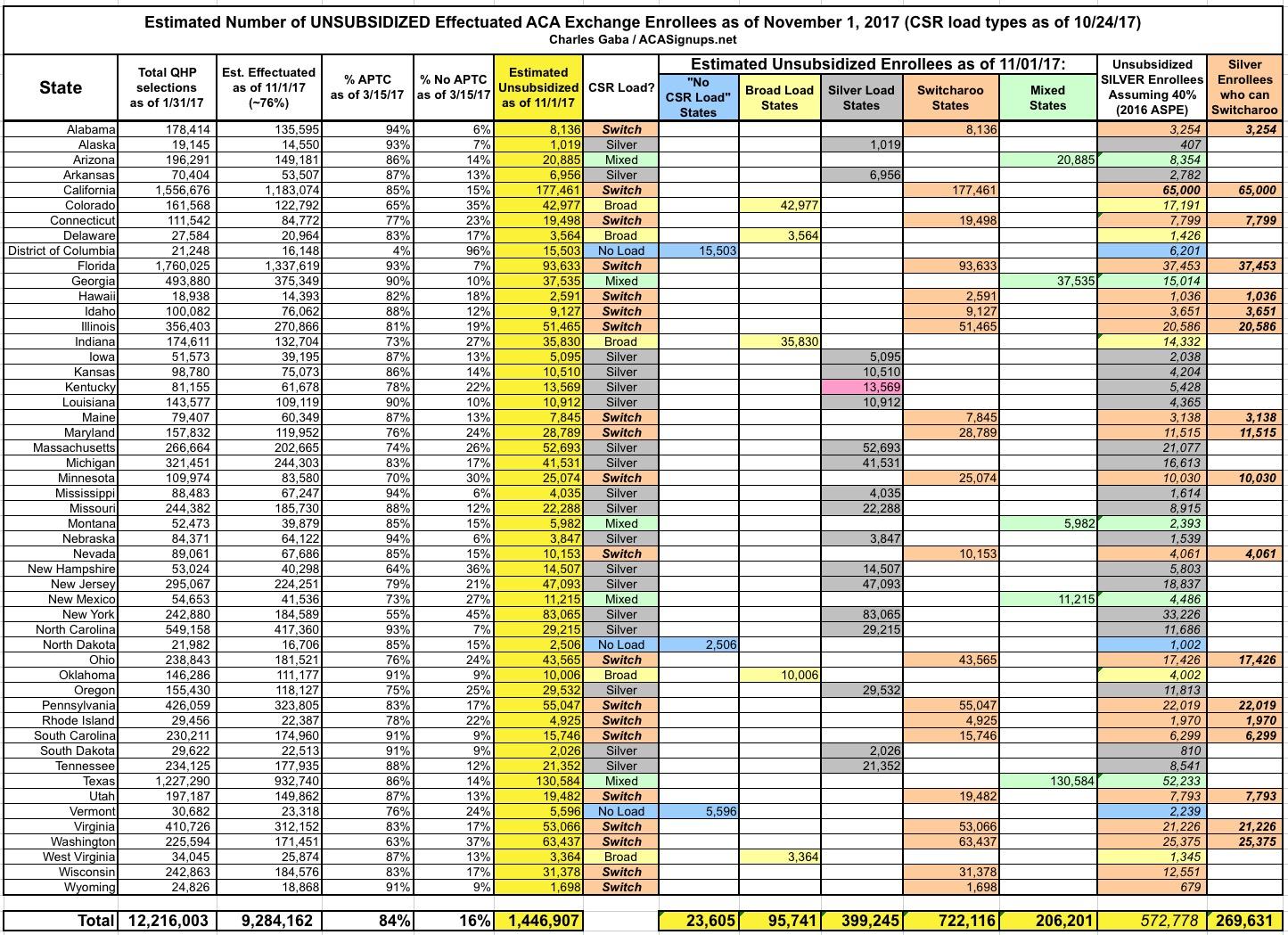
OK, the first thing I need to know is how many people will actually still be enrolled in effectuated policies as of November 1st. Around 12.2 million people selected policies as of January 31st, but due to people failing to pay their premiums in the first place, dropping their policies partway through the year or being kicked off for other reasons (legal residency issues, etc), there's normally a gradual net attrition throughout the year. This is partly cancelled out by off-season enrollees increasing the numbers, but there's still a net loss by the end of the year. In past years this seems to have averaged a retention level of around 76% as of November, which means there will likely be roughly 9.3 million people still enrolled in on-exchange policies as of November 1st.
Next: How many of those folks are unsubsidized?
Well, according to the official CMS data for the 2017 Open Enrollment Period, as of mid-March, around 84% of all exchange enrollees received APTC assistance. It's true that the March CMS report was missing about 500,000 enrollees, but proportionately that shouldn't make any difference (APTC enrollees always hover between 83-85% nationally anyway). That leaves around 16% unsubsidized, or roughly 1.45 million people total.
That gives us a table like the following, which I've also separated out by CSR Load Type to see how many people we're talking about in each category:
- Unsubsidized "No Load" enrollees shouldn't be hit with any CSR load no matter what (but these are the states most likely to change status in the next week or so)
- Unsubsidized "Broad Load" enrollees will be hit with some CSR load regardless of which ACA-compliant policy they choose to go with.
- Unsubsidized "Silver Load" enrollees will be hit with CSR load unless they switch to a Gold or Bronze plan, neither of which will have any extra CSR load included.
- Unsubsidized "Silver Switcharoo" enrollees can avoid any CSR load by switching to Gold, Bronze or an off-exchange Silver plan.
However, there's one more thing to keep in mind about "Switcharoo" states: Not all unsubsidized exchange enrollees are in Silver plans. Some are enrolled in Bronze or Gold (a handful are even in Platinum plans, but those numbers are too small to even worry about). In order to find out how many unsubsidized folks are specifically enrolled in Silver plans (and who would thus need to switch to Bronze/Gold or Off-Exchange Silver), I took a look at the OE4 Public Use Files, which break out the 2017 Open Enrollment Data by various demographic criteria....including breaking out subsidized enrollees by Bronze and Silver (they don't list subsidized Gold/Platinum numbers, oddly, but I only need Silver anyway). Unfortunately, that particular worksheet is missing the 12 state-based exchanges, but I was able to plug in rough estimates for them.
However, Andrew Sprung has noted that while the 2017 Public Use File data I looked at suggested that it's around 59% of the total unsubsidized enrollees, the 2016 ASPE addendum report says that it was more like 40%, and that this ratio likely hasn't changed much year over year. He's made a convincing argument, so I'm going with his ~40% estimate.
Based on this, I've come up with the following:
As far as I can tell, out of about 1.45 million unsubsidized enrollees total, around 24,000 are in "No CSR Load" states; 96,000 are "Broad Load"; 399,000 are in "Silver Load" states; 722 ,000 in "Silver Switcharoo" states and 206,000 are in Mixed strategy states.
Of these, around 266,000 current unsubsidized, exchange-based ACA enrollees in Silver Switcharoo states will be able to switch to an off-exchange Silver plan (or any Bronze, Gold or Platinum plan, on or off the exchange) in order to avoid the CSR hit next year.
That all made sense, right?
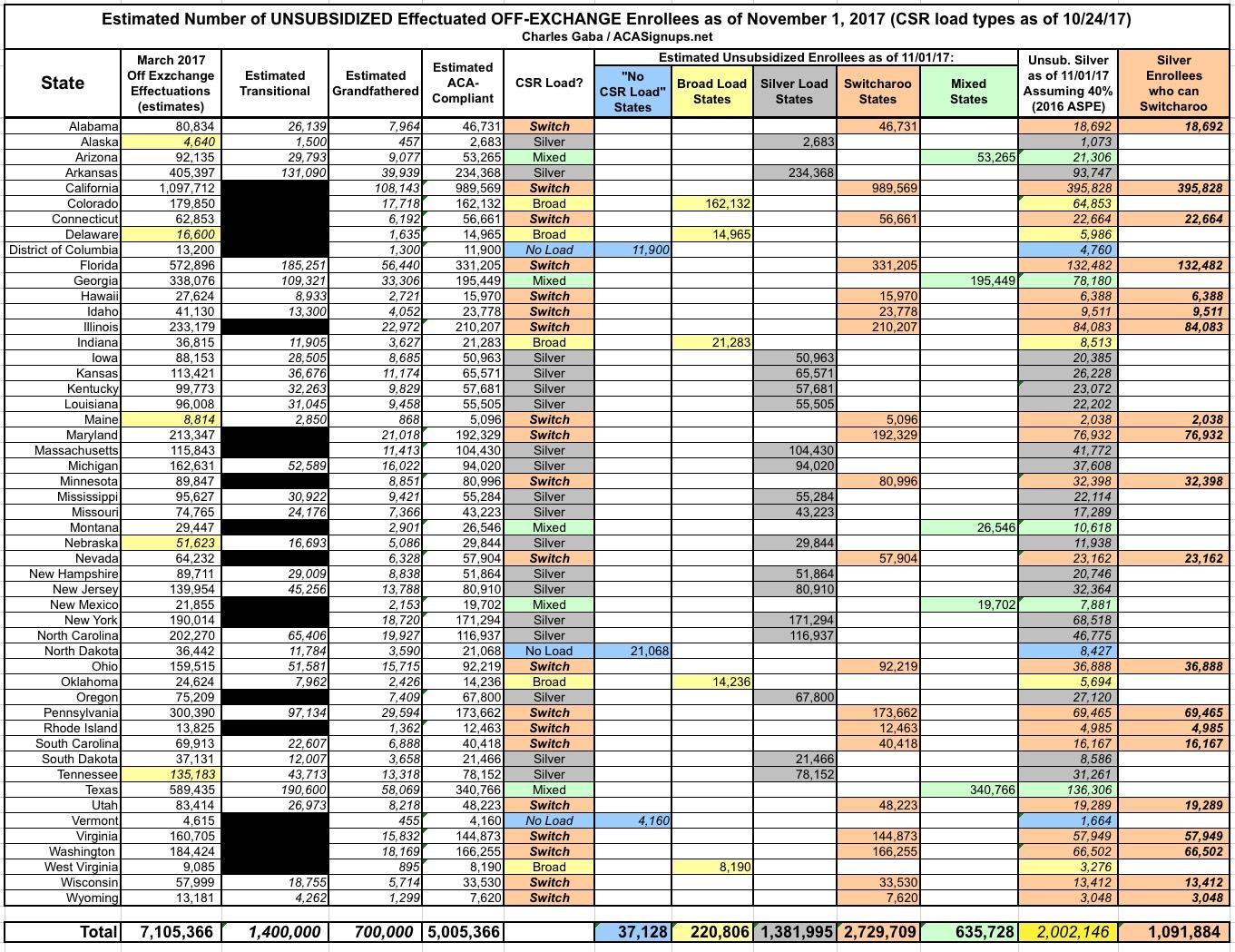
NEXT, I have to add in the off-exchange enrollees. For this, I'm relying on estimates from two respected sources: Mark Farrah Associates and the Kaiser Family Foundation.
- Mark Farrah Associates has provided their best estimates of the number of off-exchange individual market enrollees as of March 2017. I filled in a few blanks for a handful of states they were missing and came up with around 7.1 million people total.
- The Kaiser Family Foundation provides a very rough estimate of 2.1 million non-ACA compliant individual enrollees (grandfathered + transitional combined). Note that while the Axios article here gives the number as 1.2 million, I've been informed by KFF that this is a typo; it's supposed to be 2.1 million and is supposed to include both grandfathered & transitional, not just grandfathered.
Kaiser doesn't have a state-level breakout of that number, and about 1/3 of the states didn't allow (or later discontinued) tranistional plans, so I've had to run some very rough proportional guesstimates to get the following:
Again, the off-exchange numbers are very rough estimates, but assuming I'm fairly close, there should be a total of around 5.0 million people enrolled in ACA-compliant policies off-exchange.
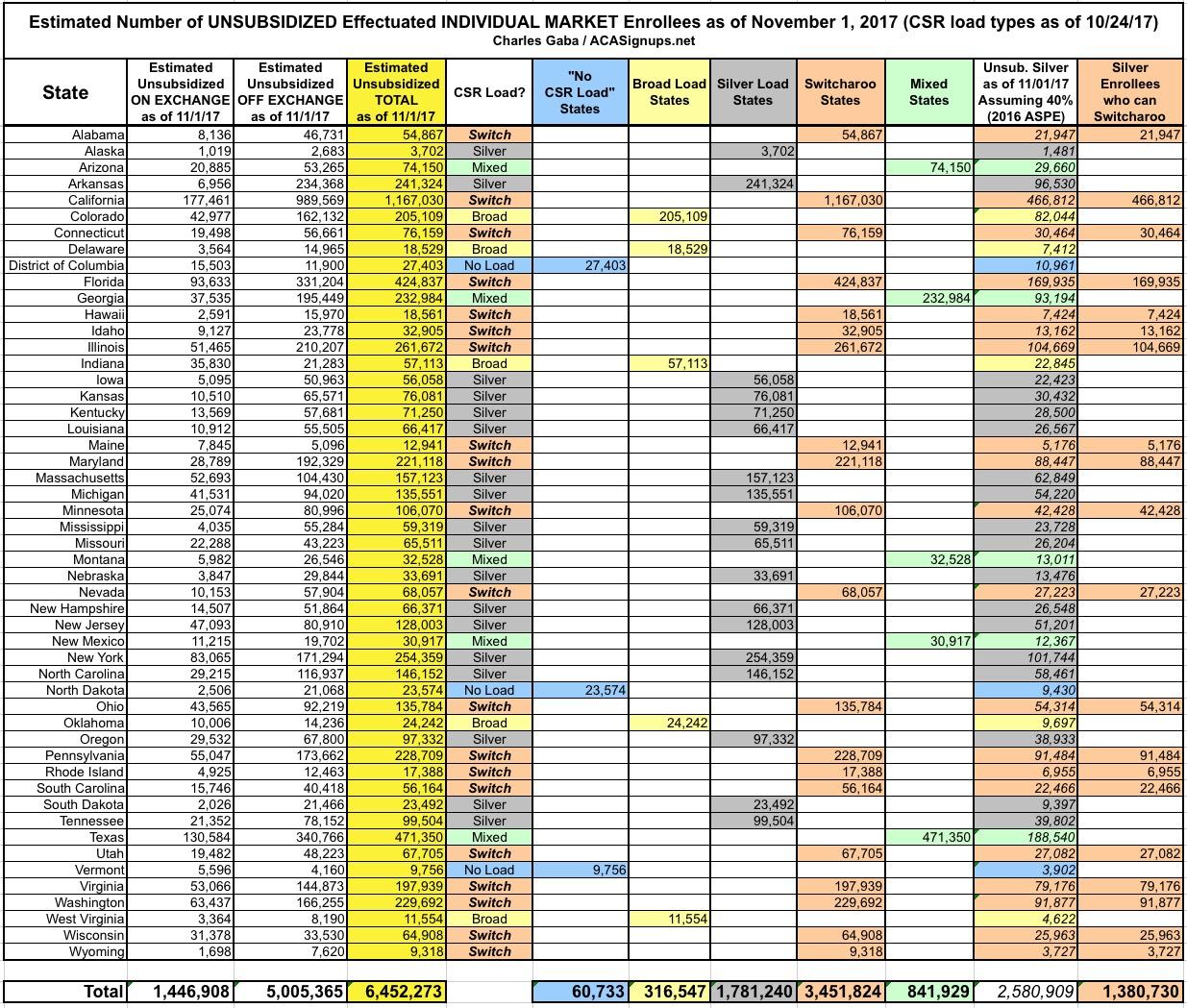
OK, now it's time to combine the ON exchange and OFF exchange numbers:
One More Time: Some of these numbers are shaky estimates, but assuming they're fairly close, the total individual market breakout (on & off-exchange combined) is roughly:
- 6.4 million unsubsidized ACA-compliant enrollees (1.4 million on exchange, 5.0 million off exchange), of which:
- 60,000 are in "No Load" states
- 316,000 are in "Broad Load" states
- 1.78 million are in "Silver Load" states
- 3.45 million are in "Silver Switcharoo" states
- 842,000 are in "Mixed" states
...and out of those 3.45 million "Silver Switcharoo" enrollees, around 1.38 million of them should be in Silver plans, which means most of them will have to switch to a different off-exchange silver (or a gold/platinum) plan to avoid the CSR hit.