UPDATED: ~10% of Medicaid Unwinding enrollees had moved to #ACA plans thru June
SEE IMPORTANT UPDATES AT BOTTOM.
Yesterday I crunched the numbers for two different reports from the Centers for Medicare & Medicaid services.
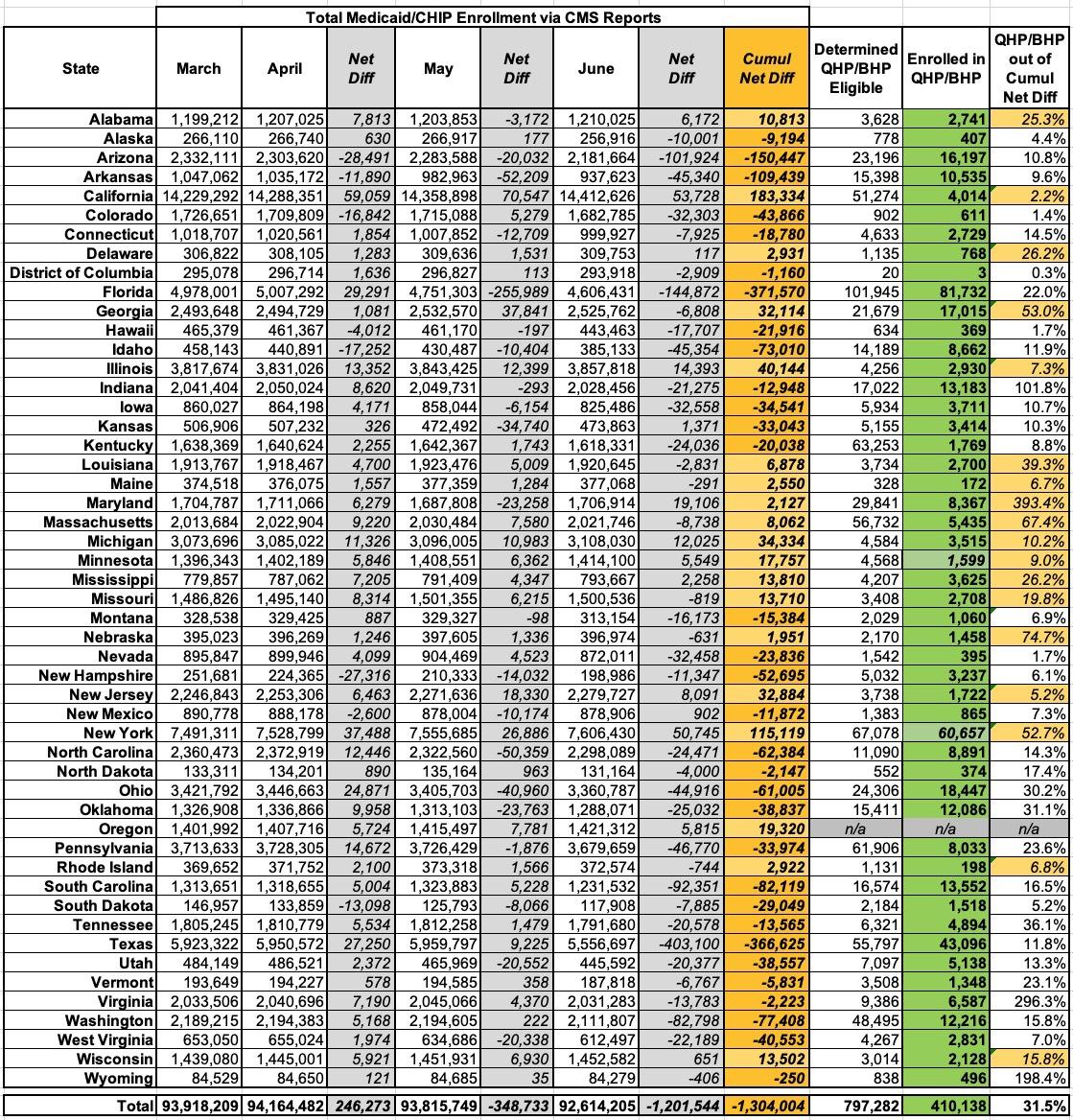
The first was the standard monthly Medicaid/CHIP enrollment report for June 2023:
In June 2023, 92,614,205 individuals were enrolled in Medicaid and CHIP.
- 85,614,581 individuals were enrolled in Medicaid in June 2023, a decrease of 1,169,095 individuals (1.3%) from May 2023.
- 6,999,624 individuals were enrolled in CHIP in June 2023, a decrease of 32,449 individuals (0.5%) from May 2023.
As of June 2023, enrollment in Medicaid and CHIP has decreased by 1,304,004 since March 2023, the final month of the Medicaid continuous enrollment condition under the Families First Coronavirus Response Act (FFCRA) and amended by the Consolidated Appropriations Act, 2023.
The second was the monthly Medicaid Unwinding data report for June 2023:
- For HC.gov, across 32 states (Oregon is missing), ~436K people who were kicked off of Medicaid/CHIP applied for ACA exchange coverage
- Of those, ~52.6K (12%) were determined by HC.gov to still be eligible for Medicaid/CHIP and presumably were re-enrolled
- The remaining ~383K (88%) were determined by HC.gov to be eligible for an ACA exchange Qualified Health Plan (QHP), with or without subsidies
- 337.2K receive subsidies; 45.5K don't
- Of those, ~291K (67% of the total who applied) actually enrolled in a QHP
The state-based exchange report is laid out little differently, but out of ~594K who applied, 414.5K were determined to be eligible for a QHP (70%); of those, only 63K actually enrolled in one, plus another 55.8K who enrolled in a BHP.
Across all states, that's 354,361 who actually enrolled in a QHP through the end of June, plus the BHP enrollees for a total of 410,138 total.
Taken at face value, this makes it look like a whopping 31.5% of the Medicaid Unwinding population (that is, people who were kicked off of Medicaid/CHIP after monthly redeterminations started up again in April) have found new healthcare coverage via an ACA exchange Qualified Health Plan (QHP) or (in Minnesota & New York only) via a Basic Health Plan (BHP).
However, other healthcare wonks I've discussed this with seem skeptical (as am I); it sounds way too high to all of us.
It's important to note that the monthly Medicaid/CHIP enrollment reports simply tally up total enrollment for that month--they don't clarify how many people left the programs (whether voluntarily or not) vs. how many new people enrolled...just the net tally. In other words, if 50,000 people lost/left Medicaid in a given state but 40,000 other people were enrolled, that would show up as a net loss of only 10,000 people.
Since Medicaid/CHIP have always had a high rate of churn (people jumping in and out each month, and sometimes in the middle of the month), it gets...messy.
As a result, I can't simply divide the 410K into 1.3M and call it a day. I decided to break the data out by state and month to see if that lends any further insight...but to be honest, it just muddies the waters even further:
As you can see above, while cumulative net Medicaid/CHIP enrollment was indeed over 1.3 million lower in June vs. March, it was actually higher in 19 states:
- Alabama, California, Delaware, Georgia, Illinois, Louisiana, Maine, Maryland, Massachusetts, Michigan, Minnesota, Mississippi, Missouri, Nebraska, New Jersey, New York, Oregon, Rhode Island, Wisconsin
There doesn't seem to be a strong pattern here, either: While most of the states have expanded Medicaid under the ACA, several haven't (Alabama, Georgia, Mississippi & Wisconsin). Eleven of the states are pretty solidly blue politically, but the other 8 are either solid red or are considered swing states.
Even in the remaining 31 states (+DC), there are three states where the number of Unwinding population members who have enrolled in QHPs/BHPs is actually higher than the state's net drop in Medicaid/CHIP enrollment (Indiana, Virginia and Wyoming).
So...I'm really not sure what to make of this data.
Having said that, if this is an accurate depiction of the situation and if that pattern has continued to hold since June, it would mean that up to 2.5 million of the 7.87 million Americans who have lost Medicaid/CHIP coverage since March have been enrolled in ACA exchange policies, which, again, sounds awfully high to me (though it would be fantastic if true).
It would also mean that an impressive 79% of those who have lost coverage (1,029,856 as of June) at least submitted their data to their state's ACA exchange in order to find out what their eligibility status was, which again sounds awfully optimistic.
Lending credence to my skepticism is this report from Washington State's HealthPlanFinder today, which states that:
- From April 1 through August 31st:
- 987,000 total Apple Health (Medicaid) customers had their eligibility redetermined:
- 572,000 (58%) remained on Apple Health.
- 415,000 (42%) customers had their Apple Health coverage end.
Of those who had their coverage end, so far:
- 88,000 (21%) are eligible for a Qualified Health Plan. Of those:
- 24,000 (6%) have selected a QHP.
- 64,000 (15%) have not selected a plan.
- 83,000 (20%) have returned to Apple Health
- 249,000 (59%) Coverage unknown. May be receiving coverage from an employer, a family member, Medicare, etc.
This report runs through August while the other reports only run through June, but on a percentage basis, the numbers for Washington State are:
- CMS reports thru June: 15.8% enrolled in QHPs (12,216 out of a net loss of 77,408)
- WA HealthPlanFinder thru August: 5.8% enrolled in QHPs (24,000 out of 415,000 who had their coverage ended)
My guess is that most states are actually closer to the latter percentage than the former. If so (around 6%), that would mean only perhaps 472,000 QHP enrollees out of the 7.87 million Unwinding population...except again, CMS says that was 410,000 had already enrolled in QHPs/BHPs through June. Huh.
I'll continue to talk to other wonks and will update this if I figure out what the true state of affairs is.
UPDATE: I discussed this with Edwin Park, a Research Professor at Georgetown University's McCourt School of Public Policy's Center for Children & Families (whew...must use a tiny font on his business cards...) who also does a lot of ACA/Medicaid data analysis. Here's a paraphrased/ summarized version of his thoughts:
- He's using a different denominator: Total Medicaid terminations for every month, which is considerably higher than either the number of those "unwound" who choose to apply to the ACA exchanges independently or who are automatically transferred over to the exchange application process by the state in question.
- In the 33 states hosted via HealthCare.Gov, only those determined to be ineligible are redirected to the exchange, not those whose eligibility is unknown. The same is true in some state-based exchange states (in fact, I already noted these in my blog post yesterday--it looks like the only exceptions are California, Connecticut, DC, Kentucky, Maryland, Massachusetts, Minnesota, New York, Rhode Island, Vermont and Washington State, which collectively only make up around 29% of the total U.S. population).
- Since procedural (red tape) terminations make up 73% of all Medicaid/CHIP terminations, that likely explains why the total is so much higher than the 1.03 million reported by the marketplace/exchange reports.
- The actual total number of Americans disenrolled from Medicaid/CHIP through June was a whopping 3.9 million, or exactly 3x higher than the 1.3 million net Medicaid enrollment drop over the second quarter of 2023.
This means that the actual QHP/BHP enrollment rate through June (410K) is more like 10.6% of the total, not 31%...which matches up much more closely with my point above about Washington State (5.8% instead of 15.8%).
Of course, this raises a different question: If 3.9 million people were kicked off of Medicaid/CHIP via the Unwinding process from April - June, but the net drop in Medicaid/CHIP coverage was only 1.3 million, what accounts for the difference? This suggests that a whopping 2.6 million other people enrolled in Medicaid/CHIP during that time period as well, cancelling out 2/3 of the terminations.
Now, this is over a 3 month period, so that would work out to an average of ~867,000 new Medicaid/CHIP enrollees per month. I suppose that's possible, but it sounds unlikely to me especially given that no states launched Medicaid expansion last spring (South Dakota didn't launch their program until July and is a tiny state anyway; North Carolina doesn't launch theirs until December).
Unfortunately, Park is at nearly as much of a loss as I am for the moment about the massive data gap here; he plans on diving into it further next week on his own blog; I'll update here when he does.
UPDATE x2: OK, in addition to the report from the Washington ACA exchange, I also found this September presentation from the Connecticut exchange (AccessHealth CT), which includes this slide:
Technical Operations & Analytics:
- 2,338 individuals enrolled in Covered CT Program*
- 5,606 individuals enrolled in a Qualified Health Plan (without a Covered CT benefit)*
- 134,760 individuals re-enrolled in Medicaid/CHIP*
- 9,798 individuals have indicated they are not requesting or are receiving health insurance elsewhere (Medicare, Employer, etc)
*Data as of August 31st, 2023
Unfortunately this doesn't tell me how many were actually disenrolled from Medicaid/CHIP, and the other report only runs through June. According to KFF's tracker, a total of 62,035 CT residents had been disenrolled via Unwinding through June, so the 2,729 QHP enrollees would have been just 4.4% of the total as of that point. It was up to 7,944 as of the end of August.
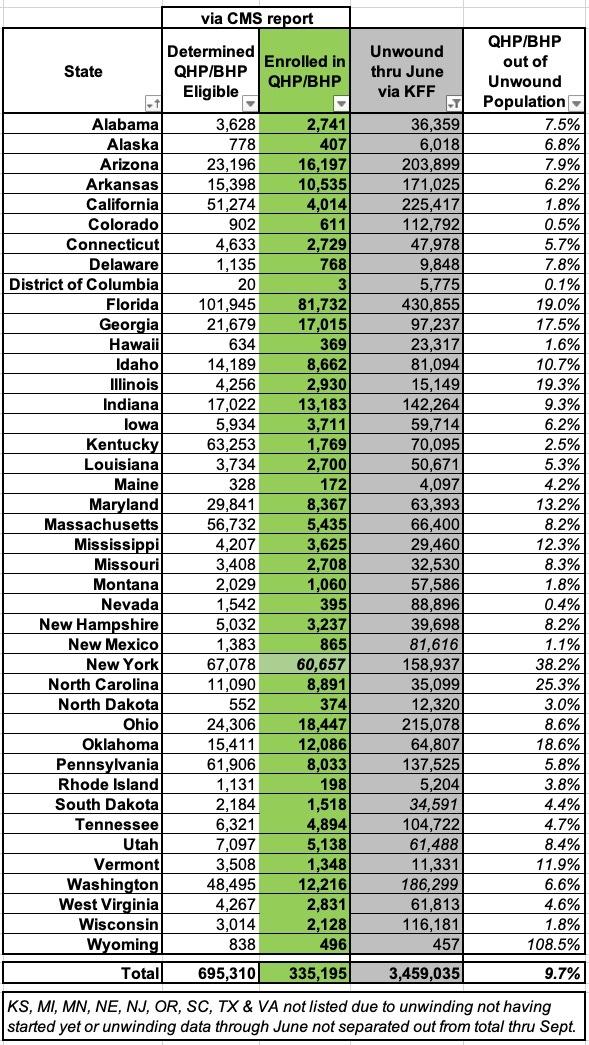
UPDATE 10/6/23: OK, I've decided to scrap the monthly Medicaid/CHIP enrollment reports entirely and go with the data from KFF's ongoing Medicaid Unwinding Tracker, which keeps a running total of how many people have actually been disenrolled from Medicaid/CHIP via the unwinding process. Their data comes directly from each state's administrative websites/reports.
Across 41 states +DC, a total of 3.46 million people had been "unwound" from Medicaid/CHIP through the end of June 2023. I'm deliberately not including 9 states because they either hadn't started the unwinding process yet as of June (Michigan, Minnesota, Oregon) or because the unwinding data for April, May & June wasn't separated out from a later report (Kansas, Nebraska, New Jersey, South Carolina, Texas & Virginia).
Across the other 41 states +DC, however, a total of 335,000 people had enrolled in QHPs (or BHPs in New York) as of the end of June, or around 9.7% of the total.
We'll see how this changes as July, August and later months are updated...
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.