Massachusetts: @HealthConnector reports 284K QHPs...*down* slightly?
Way back on November 30th (a lifetime ago!), my contact at the Massachusetts Health Connector gave me an unofficial mid-period 2021 enrollment report:
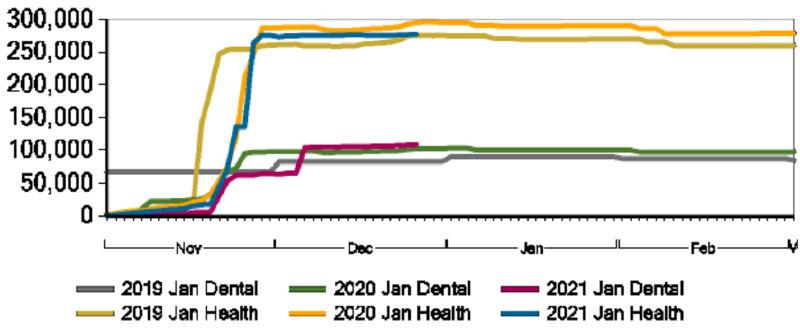
Here's where we are at, currently:
- January effectuations: 275,003
- Feb. and March effectuations: 5
- Plan Selections: 9,143
- Total enrollments: 284,151
As a reminder, "effectuations" have paid the first month premium and are good to go. Plan selections still need payment to start.
As I noted at the time, MA is one of just two states (the other is Rhode Island) which handles premium payments internally, which means they can easily track not just how many people have enrolled but how many have actually made their payments.
Yesterday I requested and received an update six weeks later, and was surprised to see the total number drop slightly:
- January effectuations: 275,020
- February and March effectuations: 3,978
- Plan selections: 4,823
- Total: 283,821
Huh. There's usually some drop-off in the state exchanges where they "front-load" auto-renewals of current enrollees, since they start out with 100% renewing and reduce it as some of those enrollees actively opt out of the renewal. Even so, you'd normally expect the total as of 1/12 to be at least somewhat higher than that of 11/30, not lower. Instead, there's a drop of 330. What's going on here?
Well, a slideshow from the Health Connector's last board meeting seems to lend some insight:
The 2021 Open Enrollment period runs from November 1 to January 23. Staff will synthesize full Open Enrollment activity after its closure but will provide an interim update today.
- Overall, halted member movement from MassHealth to the Health Connector due to the federal public health emergency has been a key reason for lower than usual enrollment
- Nevertheless, we continue to see strong activity among renewing and new members
- Staff and partners continue to work to conduct outreach, marketing, and member support on OE to maximize public and member awareness
- As of Dec. 22, 9 percent of ConnectorCare members were determined eligible for unsubsidized coverage in 2021.
- Loss of subsidies is most often due to unverified income
- While members have been slower to provide updated income information this year, it appears that bills for January have sparked a substantial number of updates over the last week
- Through Dec. 22, over 277,000 members had enrolled for January, a 6% percent reduction from last year at this time.
Lower membership is primarily the result of decreased new enrollments rather than termination of existing members, likely due to Medicaid protections associated with the federal public health emergency
Enrollments among people who were not enrolled when OE started are down about 40 percent
Overall retention remains high at nearly 94 percent, nearly identical to last year
I assume this refers to one of the provisions in the Families First COVID-19 Response Act, which put a freeze on those already enrolled in Medicaid as of March 18, 2020 (or any new enrollees) until after the public health emergency is lifted.
This is probably part of the reason, but there has to be more to it for two reasons: First, because I presume that a lot more people saw income losses than income gains last year...though I suppose the odd way in which the extended/enhanced unemployment insurance last spring were categorized for income purposes (along with the one-time $1,200 checks) did likely cause some people to see their incomes increase over the Medicaid expansion cut-off point.
The larger confusion I have about this rationale is that if it's causing this impact in Massachusetts, I would expect to see similar drops in other Medicaid expansion states. Only two other Medicaid expansion states, of those with full 2021 enrollment in, only Kentucky and Louisana saw similar year over year drops. Unless Massachusetts has some additional state-level Medicaid retention law I'm not sure why this would cause a similarly high drop in enrollment this year.
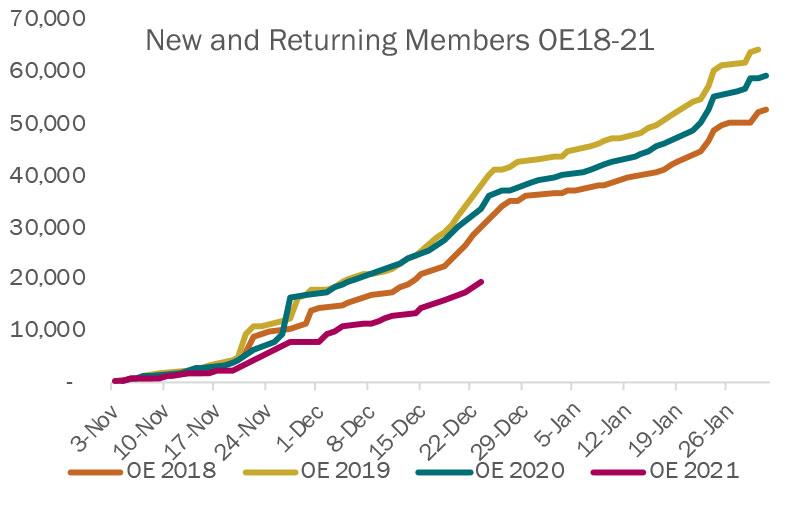
Over 55,000 renewing members and 20,000 new members have shopped so far this OE.
- This represents renewing members at all stages of the shopping process: browsing, selecting a plan, and effectuating coverage
- Even if individuals shop, they often confirm their current plan for next year
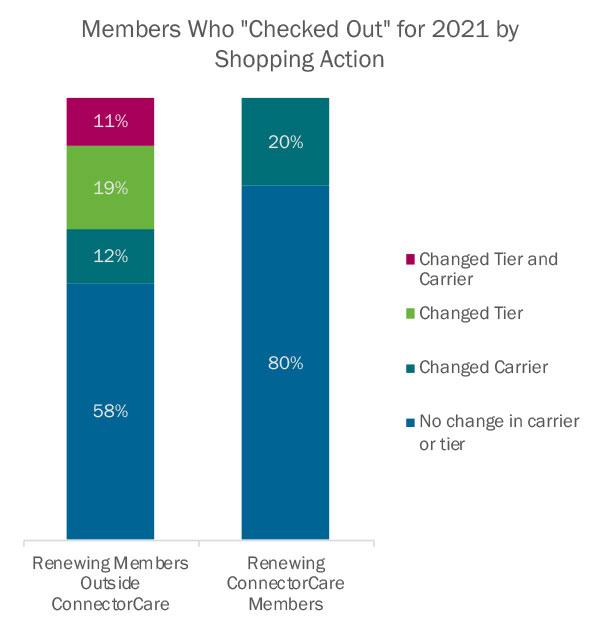
- As in prior years, members who shop generally opt for lower-cost plans
- Shifts toward Bronze have continued, with 1,400 renewing non-ConnectorCare members already having switched from a higher tier to Bronze
- 57 percent of new non-ConnectorCare enrollees chose Bronze
Last year MA ended up with nearly 320,000 people selecting Qualified Health Plans (QHPs) via their exchange, Massachusetts is around 11% behind last year's final tally, though residents still have 10 days to enroll.