What's the matter with Kansas? A lot less than before: Medicaid expansion agreement announced by Gov. Kelly & GOP leadership!
Even as I'm typing this, Democratic (!) Kansas Governor Laura Kelly and Republican legislative leaders are holding a press conference to announce an agreement to finally expand Medicaid under the ACA:
TOPEKA, Kan. (KWCH) Gov. Laura Kelly and Republican leadership announce an agreement on Medicaid expansion in Kansas.
During a press conference on Thursday, the governor said the program would be funded by the hospital administrative fee. At this time, it's unknown if that fee would be passed on to patients.
Kelly said the hospitals have endorsed the program.
Kansas Senate GOP Majority Leader Jim Denning said the bill would be pre-filed on Thursday with 22 co-sponsors.
If passed in the Kansas Senate and House, the full expansion would go into effect no later than Jan. 1.
(Obviously that's January 1st of 2021 at this point, of course)
Here's some live tweeting of the event by a Kansas-based political reporter:
There are a lot of people here for what we all expect is a deal on Medicaid expansion between Gov. Kelly and Senate Majority Leader Jim Denning. #ksleg
— Stephen Koranda (@kprkoranda) January 9, 2020
Gov. Kelly says the Medicaid expansion agreement includes parts of multiple previous Dem and GOP plans. Includes full expansion no later than Jan. 1st 2021. Paid for by a fee on hospitals. She says hospitals have endorsed it. #ksleg pic.twitter.com/HHskDTQ1ee
— Stephen Koranda (@kprkoranda) January 9, 2020
"Full expansion" presumably means none of this "only up to 100%", "money used to pay for private ACA exchange plans" or "work requirement" nonsense, which is fantastic.
Kelly says the Medicaid expansion plan includes a work referral program. #ksleg
— Stephen Koranda (@kprkoranda) January 9, 2020
A work referral program is very different from a work requirement program. Nothing wrong with including a program to help enrollees get jobs, which in turn would hopefully reduce the number of people who need to be on Medicaid (since they'd either shift to employer coverage or earn enough to be able to afford a subsidized exchange plan), as long as they're not legally required to do so to remain enrolled.
Kelly on Medicaid expansion agreement between her and Sen. Denning: "Compromise is hard, it's messy and it's slow. But it is so worth it." #ksleg
— Stephen Koranda (@kprkoranda) January 9, 2020
This is blasphemy to some quarters, of course...
Sen. Denning says Medicaid plan also includes a waiver proposal to help stabilize costs on the health care exchange. "We have a real, good, complete plan for Kansas." #ksleg pic.twitter.com/MsmrDo9TlX
— Stephen Koranda (@kprkoranda) January 9, 2020
I'm 95% sure this is referring to an ACA section 1332 reinsurance waiver, which isn't nearly as good as expanding/enhancing subsidies directly, but it's still better than nothing.
Gov. Kelly says the agreement doesn't mean Medicaid expansion is a done deal. "Ramp up your efforts and help us bring this home." #ksleg pic.twitter.com/k2k0lzfx80
— Stephen Koranda (@kprkoranda) January 9, 2020
Yep. Caution is the watchword. Kansas came within a single vote of passing Medicaid expansion a couple of years ago but it fell apart anyway. It's not done until it's done.
Denning says the Medicaid agreement has 22 Senate sponsors. It needs 21 votes to pass that chamber. "This is what governing looks like." #ksleg pic.twitter.com/AsXGQaITvY
— Stephen Koranda (@kprkoranda) January 9, 2020
The pressure on two of the Republican members to reverse themselves will be tremendous.
Denning says hospitals will pay up to $35 million in fees to pay for Medicaid expansion under the proposal. #ksleg
— Stephen Koranda (@kprkoranda) January 9, 2020
Remember, the state pays 10% of the cost, so that suggests around $350 million in total spending.
Here's the official press release from Gov. Kelly's office:
Governor, Senate Majority Leader announce compromise proposal to lower healthcare costs for Kansas families
The title of the press release alone is noteworthy...presumably the reinsurance program was included because the GOP insisted on premium reductions for middle-income residents in return for Medicaid expansion for low-income residents, and that's reasonable.
After weeks of negotiations, Democratic Governor Laura Kelly and Republican Senate Majority Leader Jim Denning today announced a compromise proposal to expand Medicaid while lowering health insurance premiums for Kansas families.
“This process is far from over, as there are still several critical steps to be taken by the Kansas Legislature,” Kelly said. “But today, Senator Denning and I are proud to stand together to propose a bipartisan compromise that will expand Medicaid and lower healthcare costs for Kansas families. This proposal includes elements of my plan, of Senator Denning’s plan, of the 2019 House plan, and of the bipartisan plan that passed both chambers in 2017.”
The compromise proposal includes key elements to address concerns raised from both parties, in both chambers:
- Full Medicaid Expansion: The proposal includes a full expansion of Medicaid to 138% of the Federal Poverty Level (FPL) with a 90/10 match, to be effective no later than January 1, 2021.
- Reinsurance: Pending Centers for Medicare and Medicaid Services (CMS) approval of a 1332 waiver and release of funding by the State Finance Council, the proposal includes a reinsurance program to be effective no later than January 1, 2022. The agreement also requires the Kansas Insurance Department to complete an actuarial study of the reinsurance proposal and submit to the State Finance Council.
Interesting...reinsurance wouldn't go into effect until 2022? Huh. I guess they think they need more time to run the numbers? I presume they can change it to 2021 if they manage to push it through quickly enough...
- Medicaid Funding: The proposal includes an annual hospital Medicaid expansion support surcharge of up to $35 million, which has been endorsed by the Kansas Hospital Association, to be effective July 1, 2021. This compromise proposal does not require a tax increase.
Heh. I mean, one person's tax is another person's fee, but still.
- Promoting Personal Responsibility: The agreement includes a robust work referral program that promotes self-reliance for non-working Medicaid beneficiaries, while limiting costly administrative red tape that drives up overall costs to taxpayers. Enrollees within the expansion population will make a modest contribution for health services through monthly premiums of up to $25 per month, or $100 for a family of four, as proposed in House Bill 2066. The bill does not contain any lockouts. Instead, it collects unpaid premiums through the state’s debt setoff program. A hardship provision is also included.
Wow...not only is Kansas not including a work requirement, the press release actually throws shade at the states which do (including my own here in Michigan, ahem...)
The "$25/mo" premium could be a problem, but the "up to" lends hope that it's on a sliding scale.
- Rural Health Care Innovations: The proposal creates an advisory committee within the Kansas Department of Health and Environment to support rural hospitals in assessing viability and identifying new delivery models, strategic partnerships and implementing financial and delivery system reform to improve the health of rural communities.
This is a big deal in heavily-rural Kansas, I presume.
“My top priority is to lower the cost of healthcare for Kansans across the board. We want to give as many Kansans health care coverage as we can, in the Medicaid market and the non-Medicaid market,” Denning said.
While this proposal is the most sweeping compromise offered since the debate over Medicaid expansion began in 2013, both Kelly and Denning underscored that more work remains.
“We’ll both be working with our respective caucuses in the coming days to get their feedback and buy-in,” Denning said. “But all sides can find something in this bill to like. That means it’s probably about as middle of the road as it can get."
“This compromise was an important first step, but our work is not over yet,” Kelly said. “Legislators, many of whom were here today, have the ability to bring this over the finish line in the early days of the 2020 session. I am calling on them to do just that.”
Here's a more detailed version:
Bipartisan Medicaid Expansion Bill Summary
New Section 2 – Full Expansion, Reinsurance Program
- Full Medicaid Expansion up to 138% FPL with 90/10 match to begin no later than January 1, 2021. This provision is separate from the reinsurance program and is not dependent on approval of reinsurance.
- The Kansas Insurance Department will complete a reinsurance waiver and an actuarial study to be submitted to the State Finance Council for approval. If approved by the State Finance Council, the Insurance Department will submit the reinsurance waiver to the Centers for Medicare and Medicaid Services (CMS).
- The reinsurance waiver will be accompanied by an 1115 waiver that would request approval from CMS to transition the 100-138% FPL population from Medicaid to the Exchange. If both waivers are approved, the reinsurance program and the 1115 waiver will be implemented no later than January 1, 2022. If CMS denies either the 1332 or the 1115 waiver, full Medicaid expansion will continue as implemented on January 1, 2021.
On the one hand, this sounds a bit backwards, since current 100-138% FPL enrollees on the ACA exchange would be shifted to Medicaid, but this is an additional waiver request which would--if approved--shift them right back onto the ACA exchange a year later, resulting in Kansas going to a partial-expansion status (Medicaid up to 100% FPL; subsidized ACA policies over that). Not likely to happen but probably necessary to get the GOP on board.
New Section 3 – Work Referral Program
- The work referral program requires an evaluation to be done by the Secretary of the Kansas Department of Health and Environment (KDHE) based on the following questions being added to the Medicaid application (requires CMS approval):
What best describes your current employment situation?
(If you select option 5, go to the next question. Otherwise skip the next question)
- I have a job (jobs) and work 20 or more hours per week.
- I have a job (jobs) and work less than 20 hours per week.
- I recently lost my job and am looking for another.
- I recently lost my job and am not currently looking for another.
- My current situation does not let me have a job (go to next question if you select this answer).
What about your current situation does not let you have a job?
- I don’t have a high school diploma or G.E.D.
- I don’t have transportation to get to a job.
- I need to care for older people in my home.
- I need to care for young children in my home.
- I need to care for someone with a disability in my home.
- I do not feel that I am healthy enough to work.
- I am a full-time student.
- The answers to those questions will go through the KEES program and used to determine who should be referred to the KansasWorks program. The KansasWorks program will maintain a unique identifier for these individuals so reports can be made to the legislature on how many individuals gain employment through this program after referral.
New Section 4 – Premiums and Debt Setoff Program
- The Secretary of KDHE shall charge individuals between 100-138% FPL a monthly premium not to exceed $25 per person or $100 per family. Unpaid premiums do not result in lockouts. Instead, they are collected through the established debt setoff program. KDHE will also be allowed to grant hardship exceptions based on criteria set by the Secretary of KDHE.
OK, the $25/mo premium is a problem, as it will actually cost more for many enrollees in this income bracket than they're currently paying for subsidized ACA exchange plans. HOWEVER, a) it says "up to" so it's possible that they'll knock it down a bit; and b) no one will be locked out of the program for a failure to pay--Kansas apparently has a "debt setoff program"
The Setoff Program is governed by K.S.A. 75-6201 et seq. and began in early 1981 following legislation that allowed the Department of Administration to set off monies the State of Kansas owes vendors and individuals against debts those entities owe to the State of Kansas. In 1993, this benefit also became available to municipalities and in 1996 for the district courts. Participation in the Setoff Program is voluntary. State agencies and district courts can immediately begin submitting debts while municipalities must enter into a written agreement with the Setoff Program (see Municipal Agreement below). Agencies submitting debts to Setoff are referred to as the Creditor Agencies.
The idea appears to be that if you're on Medicaid for a year or two and rack up, say, $600 in unpaid premiums, you can delay payment of that until you're in better financial shape and have the ability to pay it later on. Not ideal but a LOT better than work requirements and lockout periods.
New Section 5 – Premium Assistance
- Allows KDHE to implement a Premium Assistance program, whereby a certain subset of the Expansion population who has access to commercial insurance through an employer can have the majority of their premium paid for by the Medicaid agency. A cost effectiveness evaluation is performed for any group health insurance policy that is known to be available for the benefit of a Medicaid beneficiary. All information received is evaluated to determine whether or not a particular insurance policy is cost-effective for Kansas Medicaid to buy.
New Section 6 – Privilege Fee and MCOs
- This provision requires the Secretary of KDHE to assess a privilege fee for purposes of operating the managed care delivery system. • It also precludes the Secretary of KDHE from giving favorable or unfavorable treatment to for-profit or notfor-profit entities, give preference to entities that provide health insurance through the health benefit exchange, and require entities providing services to provide tiered benefit plans with enhanced benefits for individuals who demonstrate healthy behaviors by July 1, 2022.
New Section 7 & 8 – Poison Pill and Non-Severability
- Provides that if the federal match drops below 90%, Medicaid expansion shall terminate. This provision is non-severable from the remainder of the act. All other provisions are severable. New Section 9 – Privilege Fee and Expansion Privilege Fee Fund • Requires all moneys received as a product of the privilege fee specific to the Expansion population to be deposited into a new fee fund. The fund will be used strictly to offset the operating costs of Medicaid Expansion; these funds will be tracked separately from the current privilege fee, and the total receipts will be reported to the legislature each year.
This is completely reasonable. One of the official reasons a lot of states refused to expand Medicaid in earlier years (whether that was the real reason or not) is that they claimed to fear a bait & switch--that the ACA would be revised to change the 90/10 split to 80/20 or whatever, which would double the portion the state has to chip in. Having a failsafe clause isn't out of line.
New Section 10 & 12 – Cost Savings Report from KDHE
- Requires the Secretary of KDHE to submit reports to the legislature summarizing cost savings achieved by moving covered individuals from the MediKan program to coverage under Medicaid Expansion and additional revenues generated by Medicaid Expansion.
New Section 11 – Inmate Coverage for Counties
- Requires the Secretary of Corrections, upon request from County Sheriffs, to assist with ensuring county inmates receiving outside medical treatment are covered by Medicaid.
This is a big cost savings for many states and counties, which otherwise have to foot the healthcare bill for inmates themselves. Now 90% of their costs are being pushed to the feds.
New Section 13 – Legislative Post Audit
Requires Legislative Post Audit to complete an economic impact analysis of Medicaid Expansion within the first two years of expansion.
New Section 14 – Drug Rebates
- Effective July 1, 2021, requires KDHE to deposit all moneys received from drug rebates for the entire Medicaid program into the SGF, as opposed to depositing those moneys into their medical assistance fee fund, which is current practice. KDHE will be required to certify the amount of drug rebates received from the Medicaid program, and this will be a separate line item on a monthly report to the legislature. This money will be used to fund caseload estimates. This section mirrors the contents of SB231 from the 2019 session.
New Section 15 – Medical Assistance Percentage Stabilization Fund
- Creates a fund that will be used to mitigate the impact that fluctuating Federal matching rates have on SGF from year to year. The start-up capital for this fund will be any recoveries from civil action that Kansas is a plaintiff in (Texas v. United States, no. 7:15-cv-00151-O. Beginning in SFY21, any time that the Federal matching rates increase, there will be a deposit from SGF into this fund in the amount that the State would otherwise be “saving” for Title XIX expenses. In years that the Federal matching rate decreases, funds will be transferred out of this account into the SGF to offset the increased caseload costs for Title XIX. This section mirrors the contents of SB2 from the 2019 session.
New Section 16 – Rural Healthcare
- The proposal creates an advisory committee within the Kansas Department of Health and Environment to support rural hospitals in assessing viability and identifying new delivery models, strategic partnerships and implementing financial and delivery system reform to improve the health of rural communities.
New Section 17 – Kansas Insurance Department Reporting
Requires the Insurance Department to analyze and provide a report to the legislature on any cost shifting from hospitals to commercial health insurance plans as a result of implementation of the Kansas innovative solutions for affordable healthcare act.
New Section 18 – Study of State Based Exchange
Requires the Insurance Department to make expenditures to (1) study risks and benefits associated with converting the health benefit exchange operated in Kansas under the federal patient protection and affordable care act from a federally facilitated exchange to a state-based exchange, (2) hire a contractor to facilitate such study and report findings of such study to legislature no later than January 11, 2021.
WHOA! I missed this element yesterday...it's just a study of course, and the timing of it means that Kansas would likely move to a partial state exchange for 2022 and a fully state-based exchange in time for the 2023 Open Enrollment Period. That's 3 years off, but still...
New Section 19 – Uncompensated Care Task Force
- Creates an uncompensated care task force within KDHE in coordination with the Kansas Hospital Association, Kansas Medical Society, Community Care Network of Kansas and other private stakeholders to develop a plan to measure and report uncompensated care incurred in Kansas.
Section 20 – Insurance Department
- Requires the Insurance Department to make expenditures to (1) study risks and benefits associated with converting the health benefit exchange operated in Kansas under the federal patient protection and affordable care act from a federally facilitated exchange to a state-based exchange, (2) hire a contractor to facilitate such study and report findings of such study to legislature no later than January 11, 2021.
This is basically just restating Section 18 in a different way; not sure why it's necessary to mention twice but (shrug)
- Requires the Insurance Department to develop a 1332 waiver, complete an actuarial study and submit to state finance council for approval within 150 days of the effective date of the act.
Section 21 – KDHE Division Healthcare Finance
- Requires KDHE to submit a plan to CMS to implement the IMD exclusion that is in the 1115 waiver. KDHE will partner with KDADS on the mechanics of the working plan and will submit to CMS for approval by 01/01/21.
Section 22 – State Finance Council
- Appropriates $35 million to the State Finance Council in FY 2022 for the reinsurance program.
Section 23 – KanCare Oversight Committee
- Adds an extra day to the KanCare Oversight Committee to review expansion population.
Section 24 – Privilege Fee
- Cleans up the language from the existing privilege fee statute. Maintains the current privilege fee at 5.77% for all HMOs in the State.
Section 25 through 32 – Annual Hospital Medicaid Expansion Support Surcharge
- Creates an assessment to begin on July 1, 2021 to be collected and remitted to the state for purposes of funding Medicaid Expansion. The funding is capped at $35 million annually. This assessment includes The University of Kansas Health System.
Section 33 – Technical Clean-up
- Repeals certain statutes.
Section 34 – Effective Date
- Upon publication in the register.
UPDATE: Hah! That didn't take long...
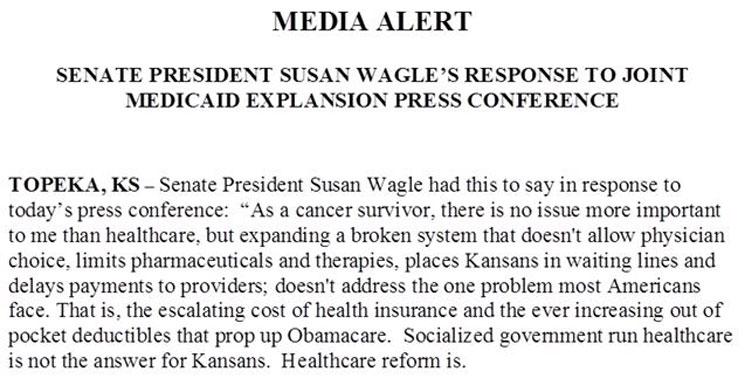
The Senate GOP is split on the new Medicaid expansion compromise. Sen President Wagle just issued a statement criticizing the agreement reached between Gov. Kelly and Senate Republican Leader Jim Denning. #ksleg
— Stephen Koranda (@kprkoranda) January 9, 2020