Massachusetts: Policyholders to receive $47 million in rebate payments thanks to 88% MLR threshold!
MLR rebate payments for 2018 are being sent out to enrollees even as I type this. The data for 2018 MLR rebates won't be officially posted for another month or so, but I've managed to acquire it early, and after a lot of number-crunching the data, I've recompiled it into an easy-to-read format.
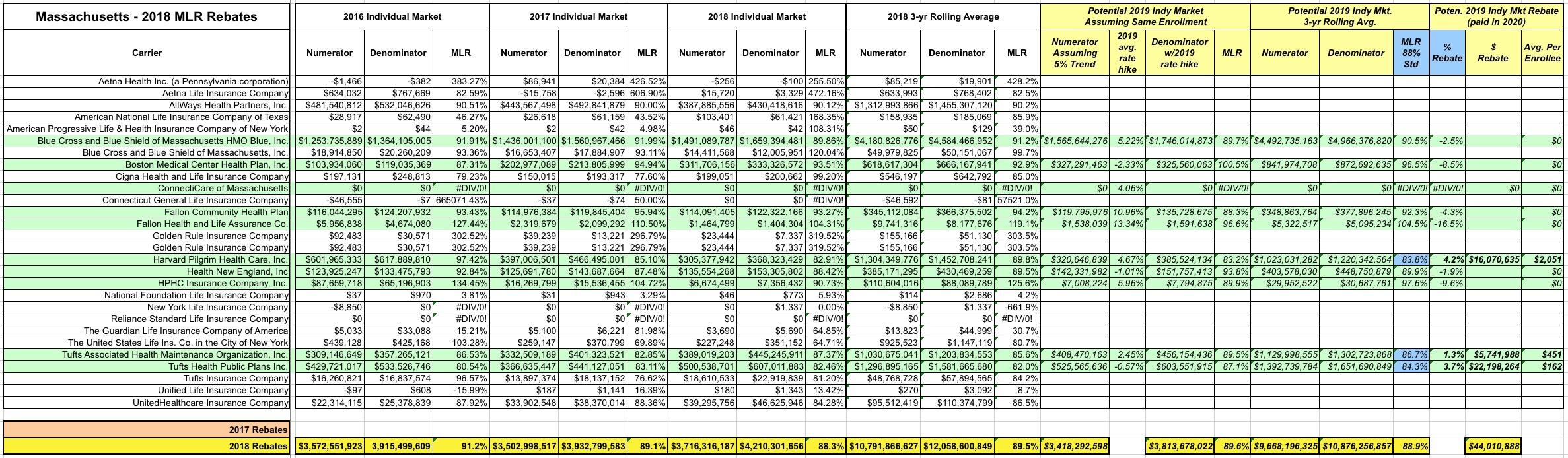
But that's not all! In addition to the actual 2018 MLR rebates, I've gone one step further and have taken an early crack at trying to figure out what 2019 MLR rebates might end up looking like next year (for the Individual Market only). In order to do this, I had to make several very large assumptions:
- First, I assumed total enrollment for each carrier remains exactly the same year over year.
- Second, I assume the average 2019 rate changes I recorded for each carrier last fall are accurate.
- Third, I assume 2019 is seeing a 5% medical trendline on average...that is, that total 2019 claims per enrollee will be 5% higher than 2018's.
All three of these are very questionable, of course, but they at least provide a baseline.
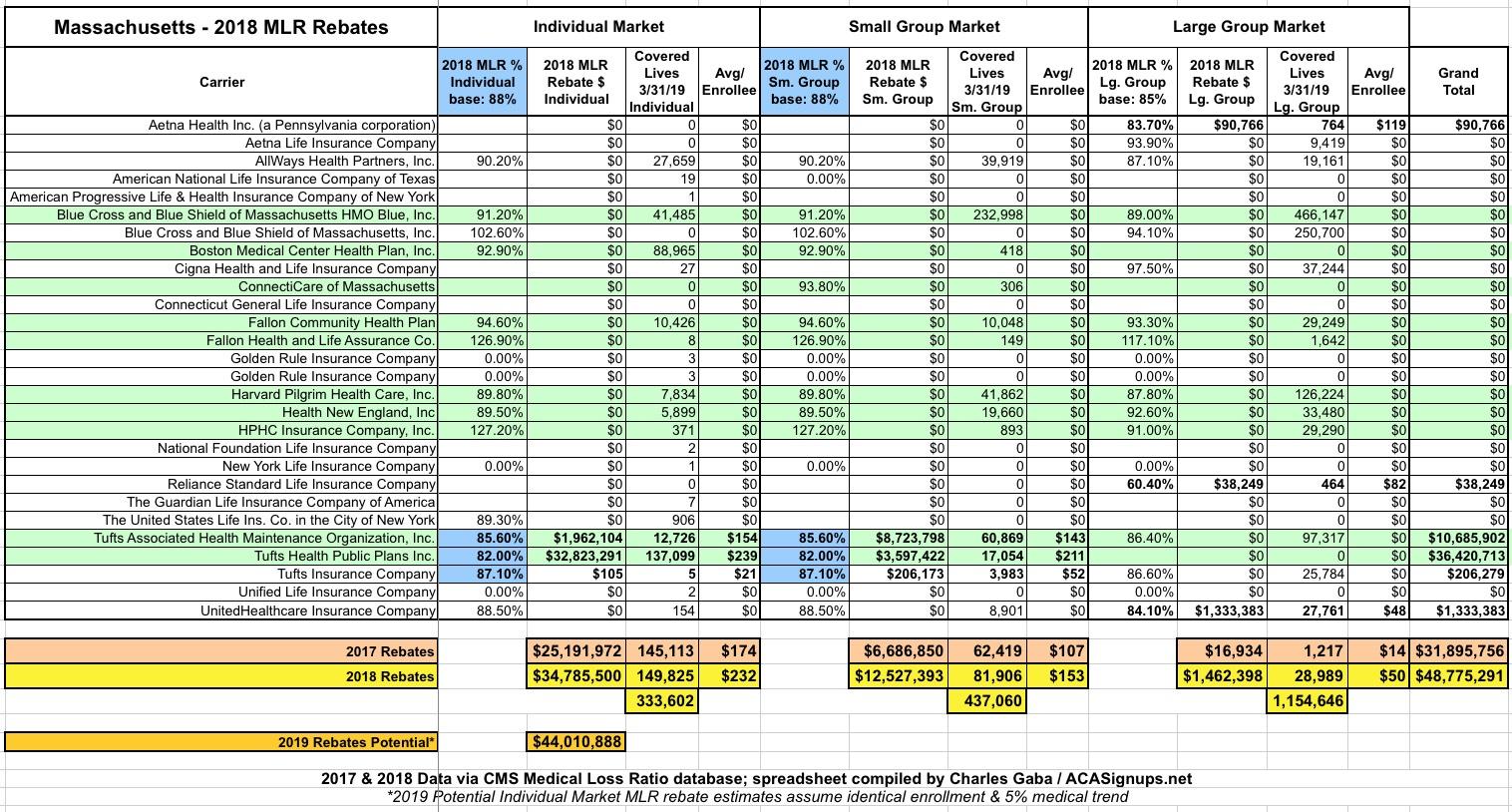
All that being said, here's what the payments for 2018 going out this month look like in Massachusetts:
WOW...I just learned something very important: Apparently not every state follows the ACA's 80% MLR rule...it turns out that at least one, Massachusetts, has a higher threshold for both the Individual and Small Group Markets:
The federal standard is lower at 80%. In Massachusetts, state law defined that the MLR for the merged individual/small group market declined from 90% in 2012 and 2013 to 89% in 2014 to 88% in 2015.
In other words, apparently up until 2012, Massachusetts set their MLR threshold at 90%, though they knocked it down 2 points since then. This is still a full 8 points higher than the federal threshold for the indy & small group markets...and as you can see above, this makes a huge difference: All $47.3 million of the 2018 Individual/Small Group market rebates is courtesy of that 8-point difference. If Massachusetts followed the same 80% cut-off as other states, enrollees would never see any of that money.
Related to this: The only serious criticism I've ever heard about the ACA's MLR rule is that it encourages carriers to collude with healthcare providers to jack up provider expenses (or at least turn the other way when providers do so), since that means they get to keep the 20% slice of an ever-bigger pie. There may be some truth to this, but it's important to note that Massachusetts has had the lowest average unsubsidized ACA premiums in the country for six years running.
In any event, due in large part to the higher 88% threshold, I expect Massachusetts to have significant Indy market MLR rebates next year as well...potentially up to $44 million:
AGAIN: There's absolutely no guarantee that things will play out this way. It's possible that none of these carriers will make MLR payments next year, or only some of them will, or the amounts will be smaller. These 2019 projections are pure speculation on my part based on a number of big assumptions.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.