Kentucky: APPROVED 2019 #ACA rate hikes: ~12.5%, but WOULD likely be FLAT w/out #ACASabotage
Hat tip to Louise Norris for the heads up about the Kentucky Dept. of Insurance issuing their final rulings for 2019 ACA individual market and small group policy premiums:
DOI Completes Review of Individual and Small-Group Health Insurance Rate Filings
The Kentucky Department of Insurance (DOI) announced today that it has completed its review of the individual and small-group insurance rates filed in the Kentucky market. The rates will be used to calculate insurance premiums in the 2019 benefit year.
Kentuckians in the individual market will once again experience changes in premiums and plan offerings. The rates that will be used reflect an average rate increase of 4.3 percent for Anthem Health Plans of Kentucky (Anthem) and 19.4 percent for CareSource. Since the actual premium charged will vary by individual and the plan level selected, some individuals may see a decrease in rates.
As Norris notes, there's some other important news regarding regional availability of carrier policies next year:
The 2019 individual market plan offerings will be expanded to additional counties. Anthem will re-enter 34 Kentucky counties, and residents in each of these counties will have a choice between Anthem and CareSource plans. Individuals in the remaining 86 counties may elect coverage by either Anthem or CareSource. Every county in Kentucky will have coverage during the 2019 benefit year. “DOI continues to explore alternatives to the Obamacare market for those individuals impacted hardest by the rate increases,” said DOI Commissioner Nancy Atkins. “However, we are pleased to have worked with our insurers to provide choices again to many individuals, and we look forward to building on that progress in the future.”
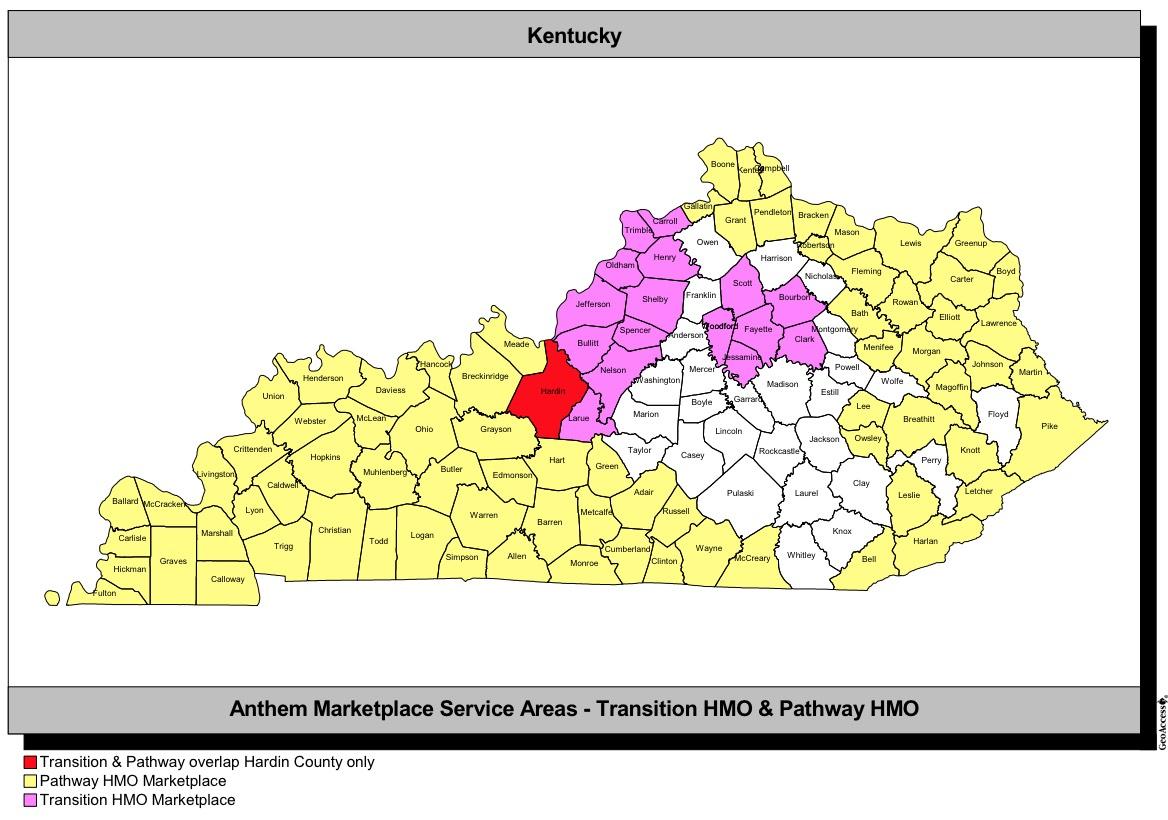
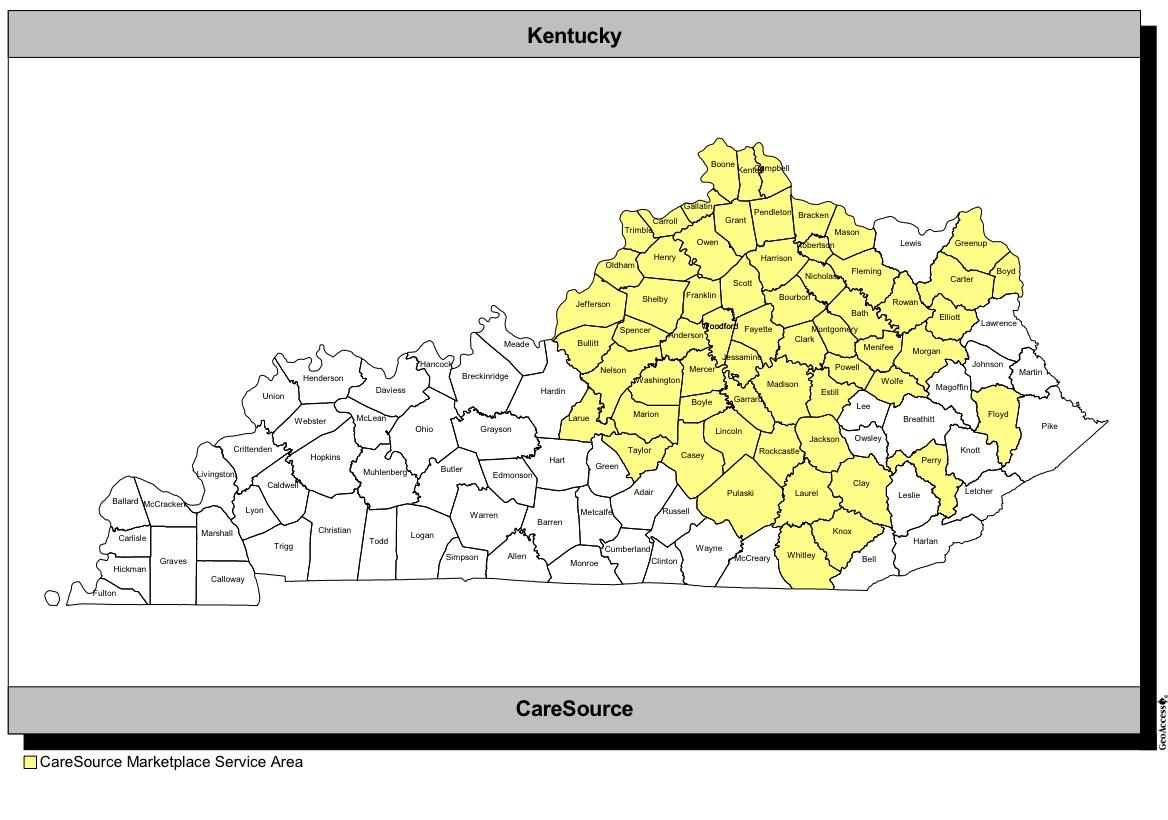
The KY DOI provides a map of which counties will be covered by which carrier next year:
Kentucky only has two carriers on the individual market, and CareSource's 19.4% rate increase was left as is. The only change was to Anthem, which actually had their average increase raised slightly, from 3.5% to 4.3%. On the other hand, they're also expanding to a bunch of states, so perhaps this makes sense depending on the demographics of the new counties they're expanding into.
CareSource notes in their filing (see below) that 5% of their 19.4% increase is due to medical/drug inflation. For the remaining 14.4%, they state flat out that the repeal of the individual mandate is a significant factor. Asuming my rough estimate of a 12.5% sabotage impact (both mandate repeal and non-ACA compliant short-term/association plan expansion) is accurate, this means that rates would have been flat year over year otherwise.