UPDATE: California: Final OE5 enrollment: 1.52M QHPs (-2.3% via Silver Switcharoo)
Note: This is more of a placeholder for the moment; it'll be updated as soon as the numbers are available.
At around 10:30am this morning, Covered California will be announcing their final, official 2018 ACA Open Enrollment Period numbers, along with other various demographic info.
Keep in mind that California is second only to Florida in terms of ACA exchange enrollees, with around 13% of the national total each year, so this is a big deal.
The most recent updates from the largest state-based exchange pegged their numbers at 1,542,000 QHP selections as of January 21st, including:
- "more than" 1.2 million renewing enrollees, and
- "more than" 342,000 new enrollees signing up.
Last year Covered CA's 1/31 total hit 1,556,676 (or just under 15,000 enrollees higher). In 2016 they had their all-time high of 1,575,340, so they'd have to have tacked on about 34,000 more over the final 10 days of Open Enrollment this year in order to beat their record.
My suspicion is that they have indeed broken through both numbers. At around noon on Wednesday the 31st, they sent out a press release stating that they were adding a 2-day "in line by midnight" overtime period for those who started their enrollment application before the midnight deadline, specifically stating that "tens of thousands" of people were expected to enroll on the final day.
At a bare minimum, "tens of thousands" equates to at least 20,000 people on the 31st alone. Add as few as another 20,000 over the prior 9 days and you're already ahead of both the 2016 and 2017 totals.
My guess is perhaps 50,000 more will be added, for a grand total of around 1.59 million people in the Golden State. I'll find out in about an hour.
UPDATE: OK, here it is...
- More than 50,000 people selected health insurance plans through Covered California in the final three days of open enrollment.
- Covered California has now served more than 3.4 million consumers since 2014.
- The number of renewing enrollees dropped slightly, in part due to Covered California encouraging unsubsidized Silver plan enrollees to shop off-exchange.
- Consumers made smart choices for 2018, picking Gold plans in many cases to get the best value for themselves and their families.
- Subsidized consumers paid less for health coverage in 2018 than 2017 due to the protective effect of their subsidy rising to offset higher premiums, while unsubsidized consumers in the individual market — both in and out of Covered California — saw their costs rise.
- Without action by Congress, unsubsidized consumers nationwide could see their costs rise steeply in 2019 and find coverage increasingly unaffordable.
SACRAMENTO, Calif. — Covered California announced Wednesday that more than 50,000 new consumers selected a plan during the final three days of open enrollment, bringing its overall total to 423,484 plan selections, which represents a 3 percent increase over last year.
Hmmmmm....that's an additional 81,484 new QHP selections, which should bring Covered CA's total up to around 1.62 million--an all-time record!
However...they also said that final renewals dropped slightly...but don't list a specific number, so it's hard to tell.
ASSUMING the renewal number still wound up at the previously-announced 1.2 million, that would indeed be roughly 1,623,484 people.
However, that's still an unknown; as noted in the press release, and as I noted yesterday in Maryland, California actively encouraged UNSUBSIDIZED SILVER ENROLLEES to move to OFF-exchange Silver policies (aka the Silver Switcharoo). They haven't released a hard number for the impact, but did say that the "dip" in renewals is "about 2%".
OK, scratch that: The "2% dip" is actually in total 2018 QHP selections; here's the official numbers:
“With robust marketing and strong partnerships in communities across California, we attracted more people to Covered California to newly enroll in health insurance this year,” said Peter V. Lee, executive director of Covered California. “Another key factor was that those getting subsidies actually had more money to shop with due to the work-around we implemented to make sure the cost-sharing reduction benefit was funded. With this increased support, we saw new and renewing consumers make smart choices, with many more opting for Gold-tier plans this year compared to last.”
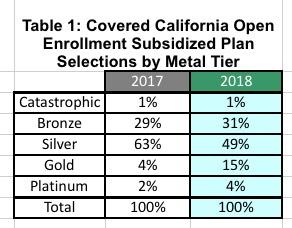
Among those who receive financial assistance, 15 percent of new consumers selected a Gold plan during open enrollment, over three times as many as the 4 percent that selected a Gold plan last year (see Table 1: Covered California Open Enrollment Subsidized Plan Selections by Metal Tier). Covered California’s Gold plans generally have higher premiums but pay 80 percent of consumers’ health care costs when they access care. Gold plans were a better value for consumers this year because the premium was lower due to the cost-sharing reduction surcharge that was added only to Silver plans.
Table 1: Covered California Open Enrollment Subsidized Plan Selections by Metal Tier
When you line up the 2017 & 2018 numbers with the metal level breakout above, here's what it looks like:
In short, it appears that perhaps 40,000 - 50,000 unsubsidized Silver enrollees were deliberately shifted to off-exchange Silver plans to avoid the CSR hit, via the Silver Switcharoo gambit. If these folks had stuck around, 2018 exchange enrollment would have slightly edged last year.
Lee said the data shows consumers are making wise choices about health insurance.
“If price were the only thing that mattered, consumers would have largely moved to Bronze-level plans, which have the lowest price,” Lee said. “But instead we saw a ‘gold rush’ of smart shopping in 2018, with consumers buying a richer benefit with their increased subsidy dollars.”
The number of new consumers selecting Platinum plans increased from 2 percent to 4 percent, while the number of consumers selecting a Bronze plan increased from 29 percent to 31 percent. Consequently, the number of new consumers selecting a Silver plan dropped from 63 percent last year to 49 percent this year.
The cost-sharing reduction “work-around” was designed to protect the hundreds of thousands of Californians who do not receive federal subsidies. One of the impacts of the cost-sharing reduction work-around was that Covered California encouraged unsubsidized enrollees who had bought Silver plans in 2017 to consider getting the comparable product off-exchange for 2018 and avoid paying the cost-sharing reduction surcharge. “While we’re still analyzing the data, it’s clear that some of the decrease in our renewals was due to consumers moving off-exchange to get coverage,” said Lee. “This fact underscores that our reports only tell part of the story of the individual market in California.”
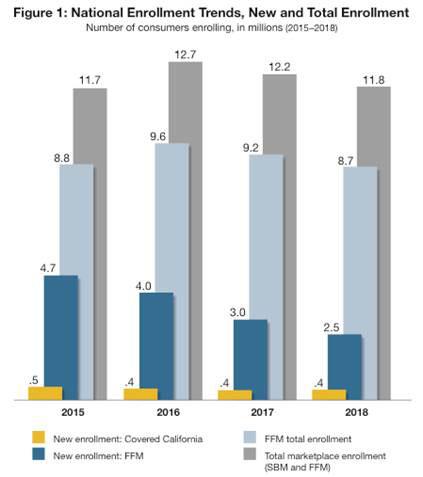
Lee also offered observations Wednesday about enrollment in the federal insurance marketplace and other state-based exchanges.
“We are seeing remarkable stability in exchanges across the nation. While the federally facilitated marketplace has seen a decline of over 10 percent since 2016, states like California that are served by state-based marketplaces have on average grown by 1.5 percent in the same period,” Lee said. “Dropping enrollment in states that rely on the federal government for marketing and outreach will directly translate to higher premiums due to the worse risk mix. With the potential dramatic rate increases likely in many states, those states that don’t have state-based marketing efforts are at risk of seeing spiraling costs for the unsubsidized, which will likely price millions out of the ability to afford insurance.”
Lee’s comments coincide with new data compiled by the National Academy for State Health Policy (NASHP) that shows that state-based marketplaces’ enrollment outpaced that of the federally facilitated marketplace.[1]
“We know that enrollment in the federal health exchange has been hampered by dramatic cuts in marketing and funding for Navigators to help people enroll,” Lee said. “Our preliminary analysis suggests there has been a dramatic drop in new enrollments in the last two years, meaning the federal exchange is not ‘refilling the bucket’ with new enrollees even though their renewals are holding steady.”
Over the past four years, the number of consumers newly enrolling in federally facilitated marketplace states has dropped from 4.7 million in 2015 to 2.5 million in 2018. In particular, in the two years that the current administration has been at least partially responsible for promoting enrollment — which included the decision to reduce marketing during the end of open enrollment for the 2017 plan year and to reduce marketing spending dramatically for 2018 — new enrollment has declined 38 percent (from 4 million in 2016 to 2.5 million in 2018). (See Fig. 1: National Enrollment Trends, New and Total Enrollment[2].)
“The problem,” Lee noted, “is that new enrollees refresh the risk mix and help keep rates down. Failing to ‘refill the bucket’ at the top — coupled with the rate increases due to ending the individual mandate — means that enrollment in the federal marketplace, and the individual market more broadly, is headed for trouble next year unless action is taken soon.”
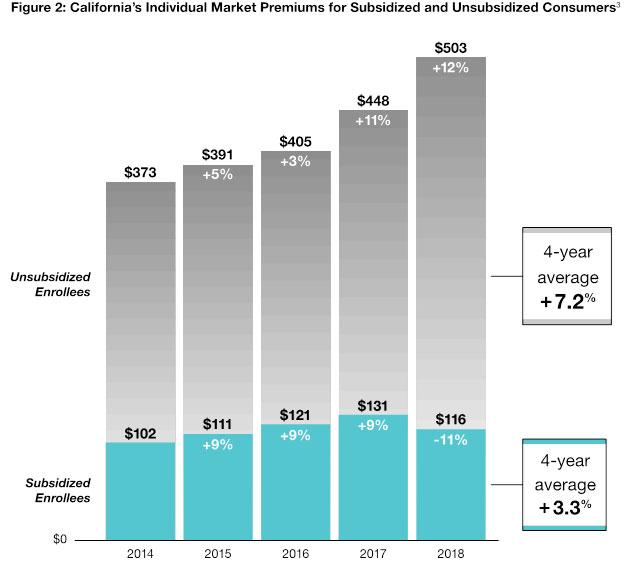
Covered California also released analysis of the premium changes for both subsidized and unsubsidized consumers over the past four years (see Fig. 2: California’s Individual Market Premiums for Subsidized and Unsubsidized Consumers, on next page).
That data confirmed how the financial subsidies are bringing health care within reach to the 85 percent of Covered California enrollees who receive subsidies — with their cost of coverage dropping 11 percent in 2018, reflecting an average monthly cost of $116.
At the same time, the data finds that for unsubsidized consumers — buying either through Covered California or directly from the same carriers in the individual market —premiums increased at an average annual rate of 7.2 percent.
“An average monthly premium of $503 can be tough for those not getting subsidies,” said Lee. “However, over the past four years we’ve kept premium increases to about 7 percent. Our efforts to enroll a healthy pool of enrollees are paying off in lower increases for those who pay the full premium.”
On Jan. 18, Covered California released a report, “The Roller Coaster for Consumers Continues: The Prospect for Individual Health Insurance Markets Nationally for 2019: Risk Factors, Uncertainty and Potential Benefits of Stabilizing Policies,” which estimates that potential premium impacts for 2019 would likely vary greatly state by state, but could be as high as 30 percent in some states.
“Those who do not get help to buy health insurance — an estimated 6 million people across the country — will not have any protection against those rate increases,” Lee said. “The unsubsidized are too often forgotten, and we know that most are middle class Americans with a median income of $75,000. Many will be priced out of coverage if premium hikes are not held in check.”
Earlier this year Covered California released a study that found the enrollment drop in 2018 nationally could have been even greater if not for a dramatic increase in the news coverage of the enrollment periods and deadlines. Ogilvy, a global leader in communications and media, was commissioned to examine coverage trends for the 2017 and 2018 open-enrollment periods across the country. The report found that mentions of “enrollment,” “enrollment period” and “deadline” increased by 53 percent, 125 percent and 129 percent respectively year over year (see Fig. 3: National News Coverage About Open Enrollment Increased Dramatically Year Over Year).
In the absence of federal or state policy changes, rate increases in California in 2019 are likely to be steep but on the “low end” of the range for states nationally due to the starting relatively healthy risk mix and Covered California’s commitment to maintaining a robust marketing campaign to attract and retain a healthy consumer pool that reduces premiums for everyone.
Lee said federal action to stabilize the individual market could make a big difference for millions of unsubsidized consumers who otherwise will face large rate increases.
Since 2014, more than 3.4 million people have purchased health insurance through Covered California, and nearly 4 million have enrolled in the state’s Medi-Cal program. Together, the gains have cut the rate of the uninsured in California from 17 percent in 2013 to a historic low of 6.8 percent as of June 2017.
Consumers can still sign up for health care coverage if they experience a life-changing event, such as losing their health insurance, getting married, having a child or moving. For more information on special-enrollment rules, visit: www.CoveredCA.com/individuals-and-families/getting-covered/special-enrol....
Eligible consumers who are interested in signing up should go to www.CoveredCA.com where they can get help to enroll. They can explore their options and find out if they qualify for financial help by using the Shop and Compare Tool. They can also get free and confidential enrollment assistance by visiting www.coveredca.com/find-help/ and searching among 800 storefronts statewide, or more than 17,000 certified enrollers who can assist consumers in understanding their choices and enrolling, including individuals who can assist in other languages. In addition, consumers can reach the Covered California service center by calling (800) 300-1506.
Consumers who qualify for Medi-Cal can enroll year-round.
[1] The NASHP report includes data as reported to the federal government, including more than 388,000 new enrollees who signed up for Covered California during the fifth open-enrollment period and 1.13 million re-enrolling consumers. Covered California reports 423,484 enrollees in order to be consistent with reporting new plan selections in each of the last five years. Not all consumers who sign up during open enrollment end up with effectuated coverage. Complete totals for effectuated enrollment are released in Covered California’s Active Member Profiles at http://hbex.coveredca.com/data-research/.
2 Data for 2015 through 2017 from Centers for Medicare and Medicaid Services, “Marketplace Open Enrollment Public Use Files”:
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Tren...
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Tren...
- https://www.cms.gov/Research-Statistics-Data-and-Systems/Statistics-Tren...
Data for 2018 from Centers for Medicare and Medicaid Services, “Final Weekly Enrollment Snapshot For 2018 Open Enrollment Period” (December 28, 2017) and equivalent state marketplace data compiled by the National Academy for State Health Policy.
3 3 Unsubsidized consumers are those who do not receive financial assistance from the federal government to pay their health insurance premiums. These consumers can purchase inside and outside of the exchange. Unsubsidized consumers in the individual market total 1.15 million, of whom roughly 1 million are in Affordable Care Act-compliant, non-grandfathered plans. See below for more detail about the unsubsidized premiums shown.
Subsidized consumers are those who receive substantial financial assistance from the federal government to pay their health insurance premiums. The Affordable Care Act requires consumers to purchase through the exchange to receive this assistance. In California, subsidized consumers total approximately 1.2 million people.
Premiums are the actual observed average premiums in Covered California administrative data for renewal and open enrollment plan selections, and the percentage change is the change to the average observed premiums. Year over year, the average premiums shown may be influenced by changes in the population distributions (such as for region, age, metal tier, etc.). Average premiums for the off-exchange market as a whole could differ from the Covered California unsubsidized premiums to the extent that the off-exchange population and plan-choice profiles differ from the on-exchange, unsubsidized profile. Additionally, the 2018 unsubsidized premiums have been adjusted to remove the cost-sharing reduction “surcharge” in Silver, since off-exchange enrollees do not incur the surcharge and Covered California encouraged its unsubsidized Silver enrollees to move off-exchange to avoid the surcharge in 2018.
How to support my healthcare wonkery:
1. Donate via ActBlue or PayPal
2. Subscribe via Substack.
3. Subscribe via Patreon.